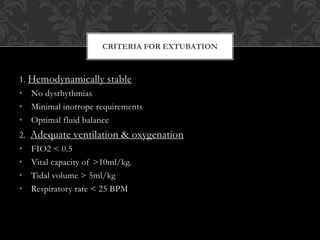
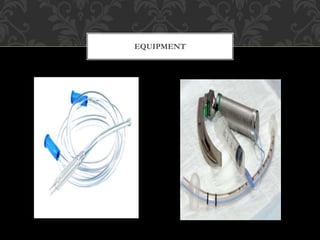
This document discusses the criteria and process for extubating a patient from mechanical ventilation. It begins by defining extubation as the removal of the endotracheal tube, which should only be done once a patient no longer requires ventilation and can protect their airway. Specific criteria are provided for assessing a patient's readiness, including hemodynamic stability, adequate oxygenation, normal blood gases, resolution of underlying conditions, and intact neurological function. Potential complications are also reviewed. The process of extubation involves preparing equipment, explaining to the patient, continuously monitoring their condition, and carefully removing the tube while suctioning and assessing airway patency.