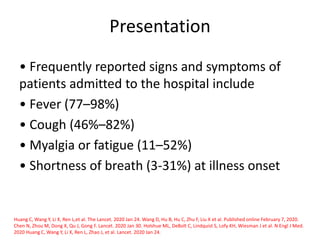
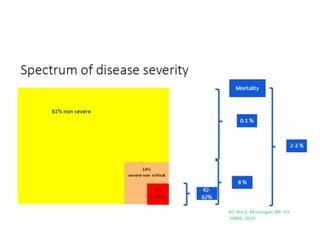
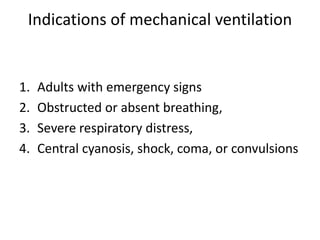
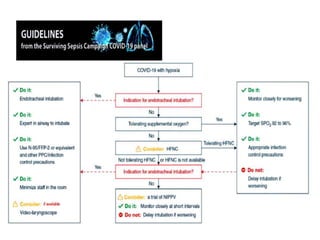
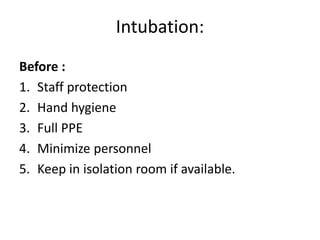
The document outlines airway management strategies for COVID-19 patients, emphasizing the need for proper protective measures and meticulous preparation for intubation. It details indications for mechanical ventilation, including severe respiratory distress and obstructed breathing, and highlights the importance of monitoring and managing potential complications. Protocols for safely managing intubation and mechanical ventilation in a COVID-19 context are outlined to ensure effective treatment while minimizing risk to healthcare workers.