This document discusses awake intubation, including:
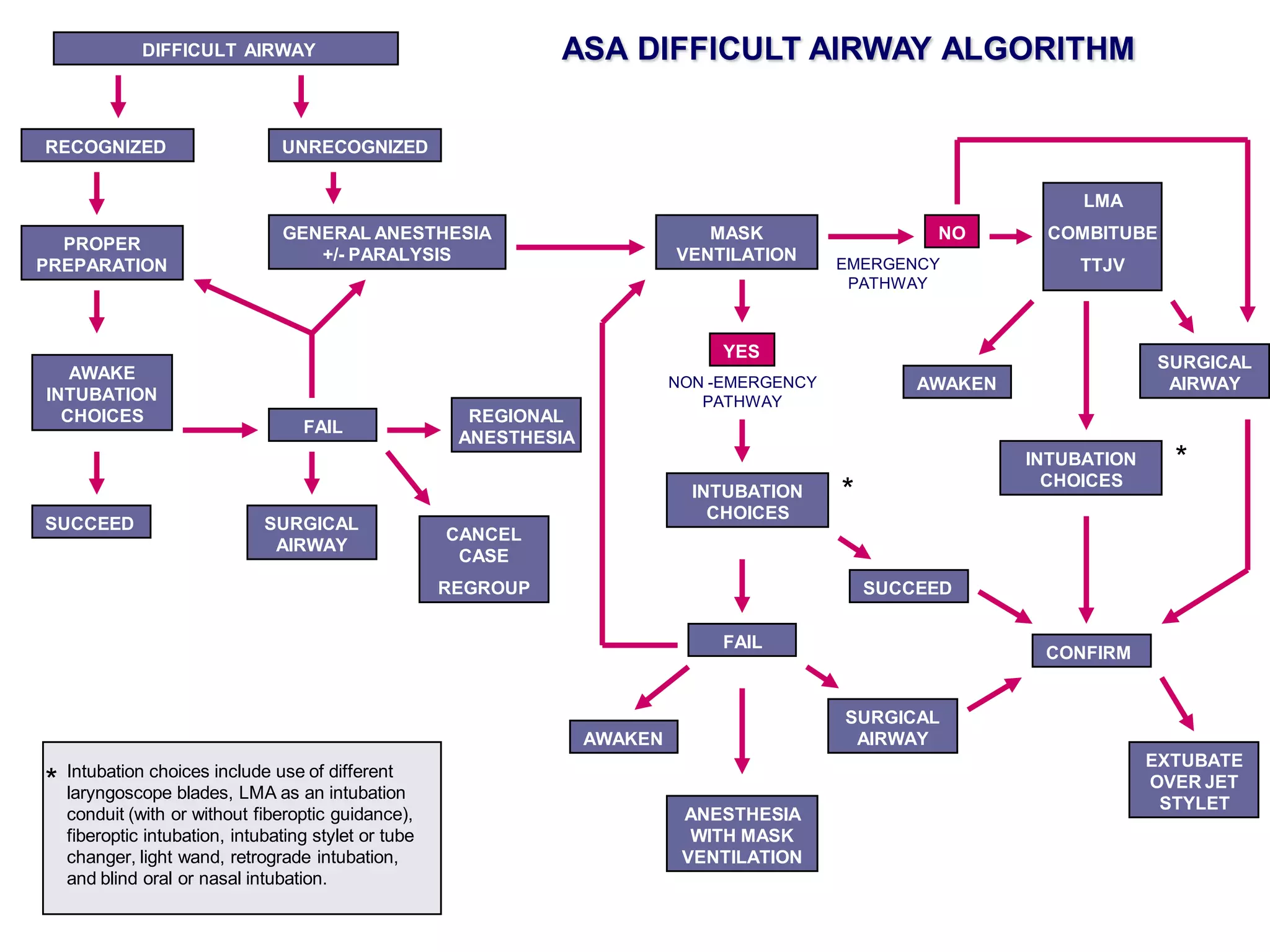
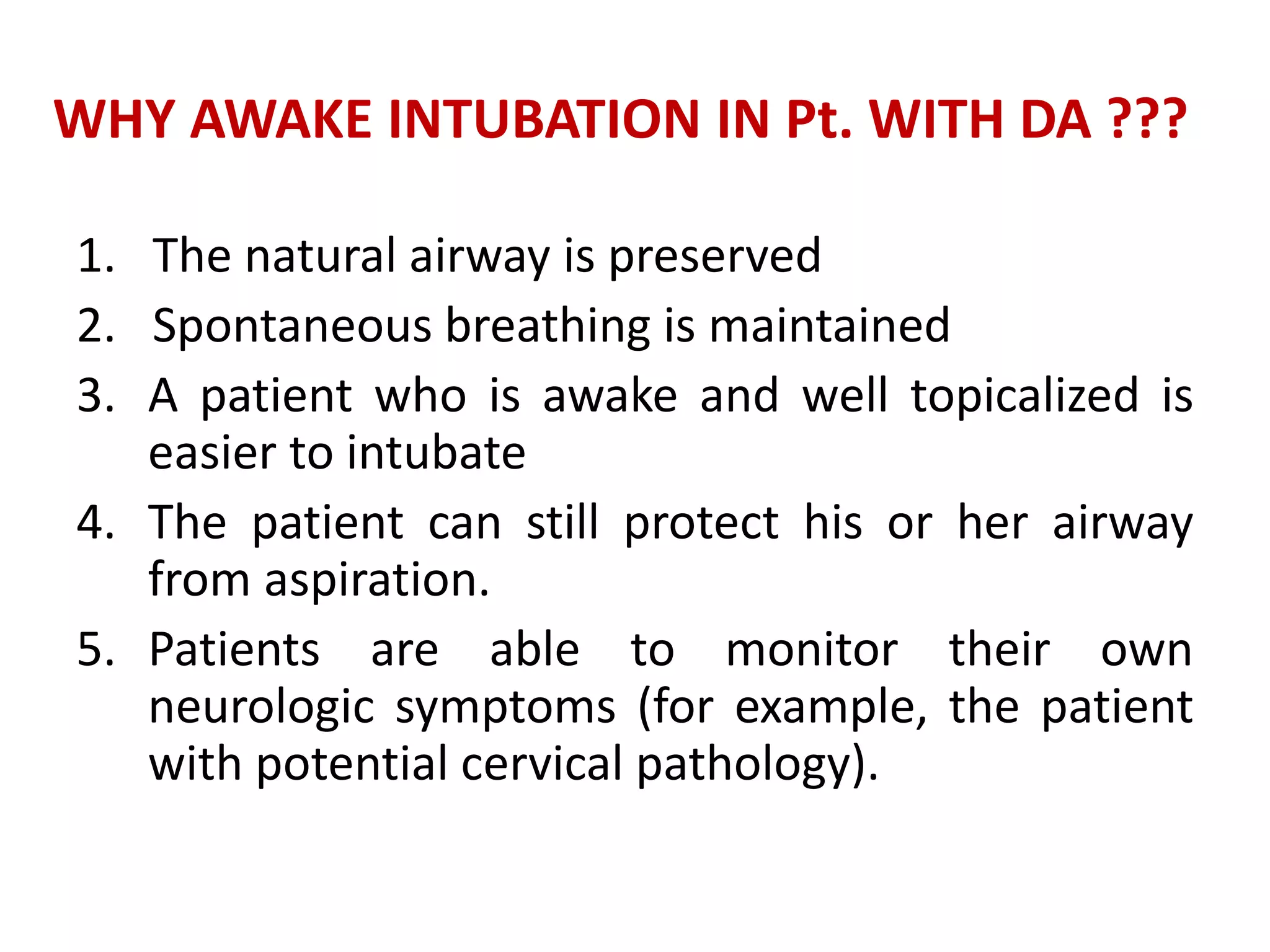
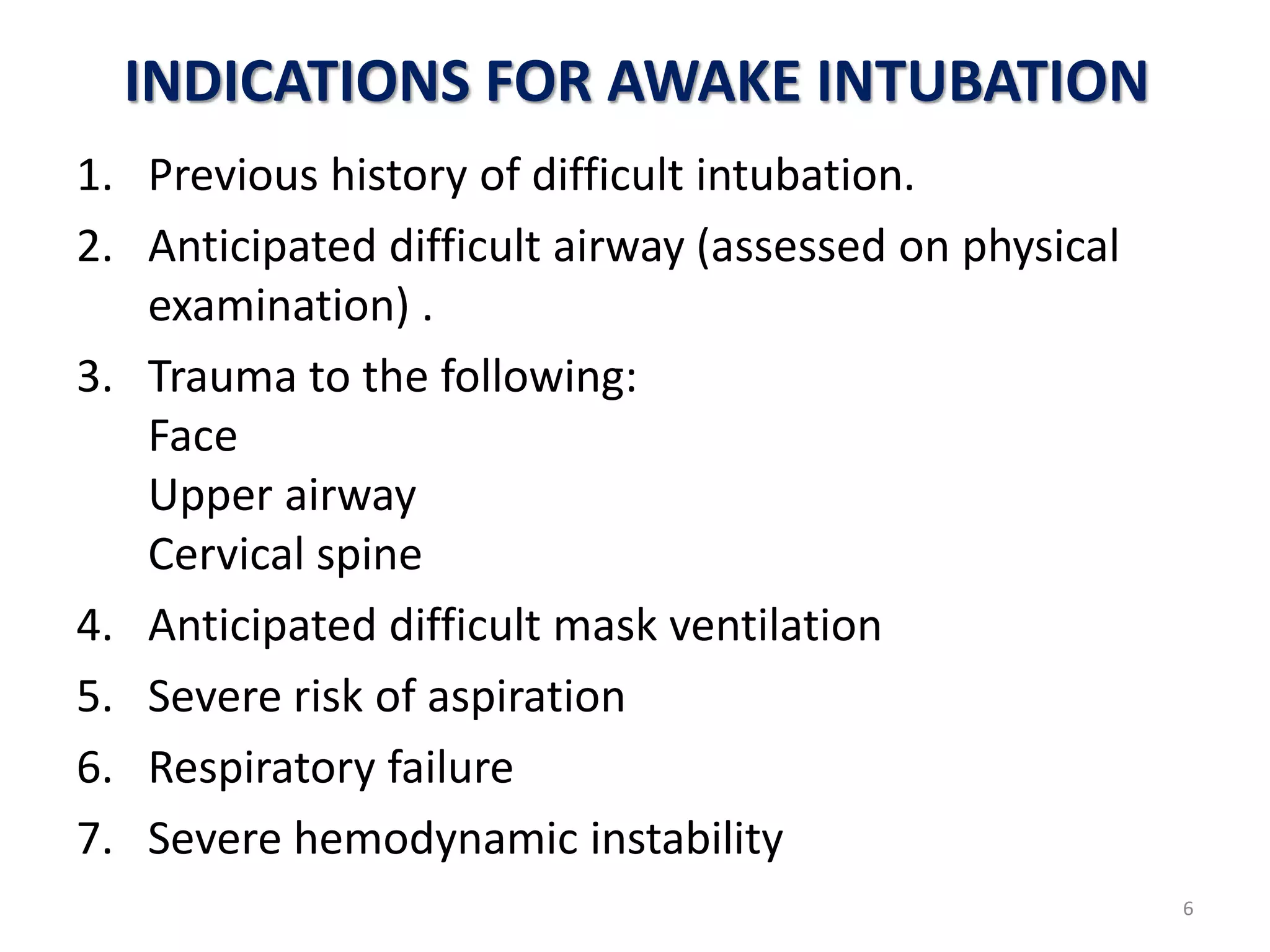
1. Awake intubation is indicated for patients with anticipated difficult airways to maintain airway patency.
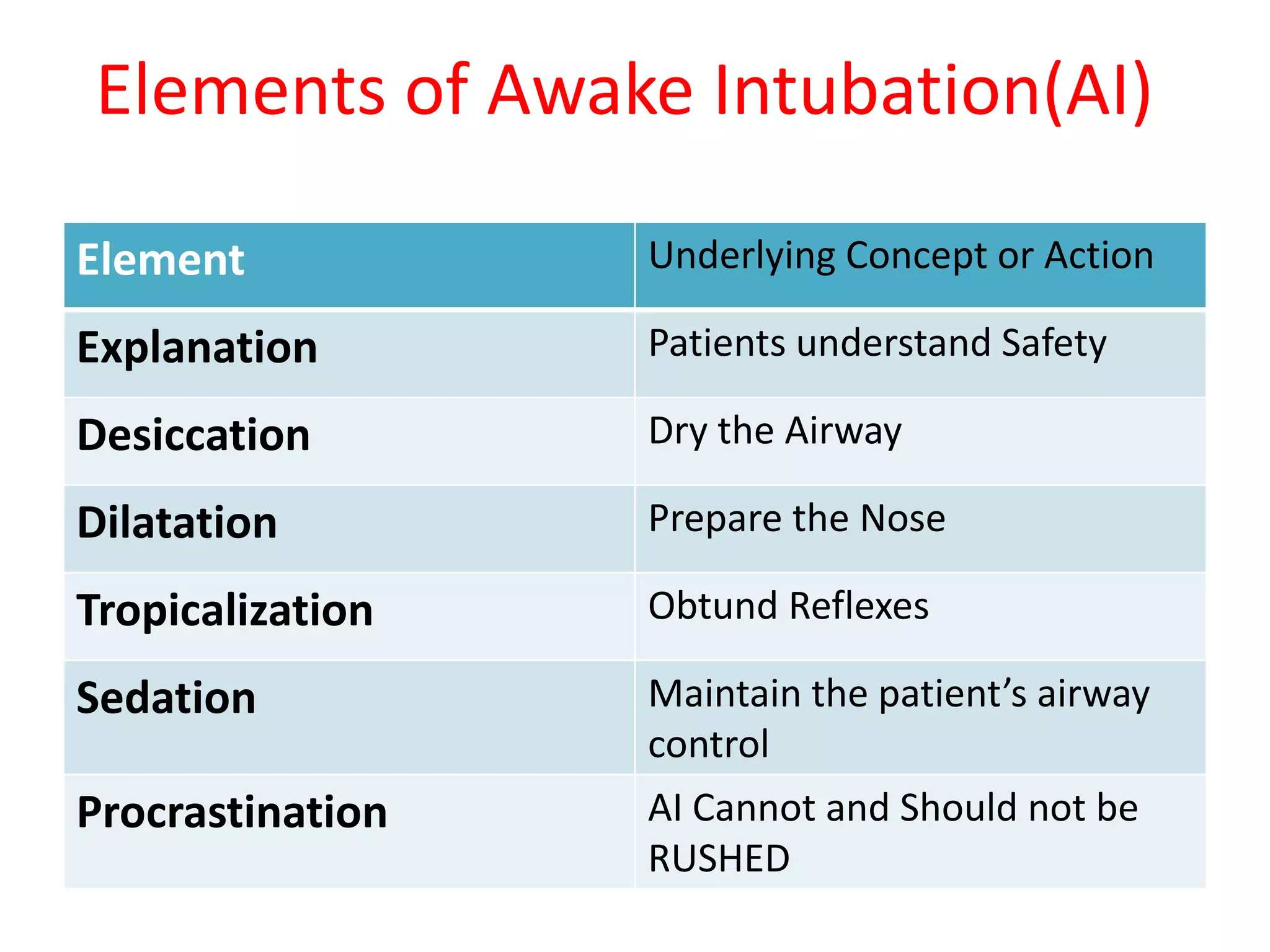
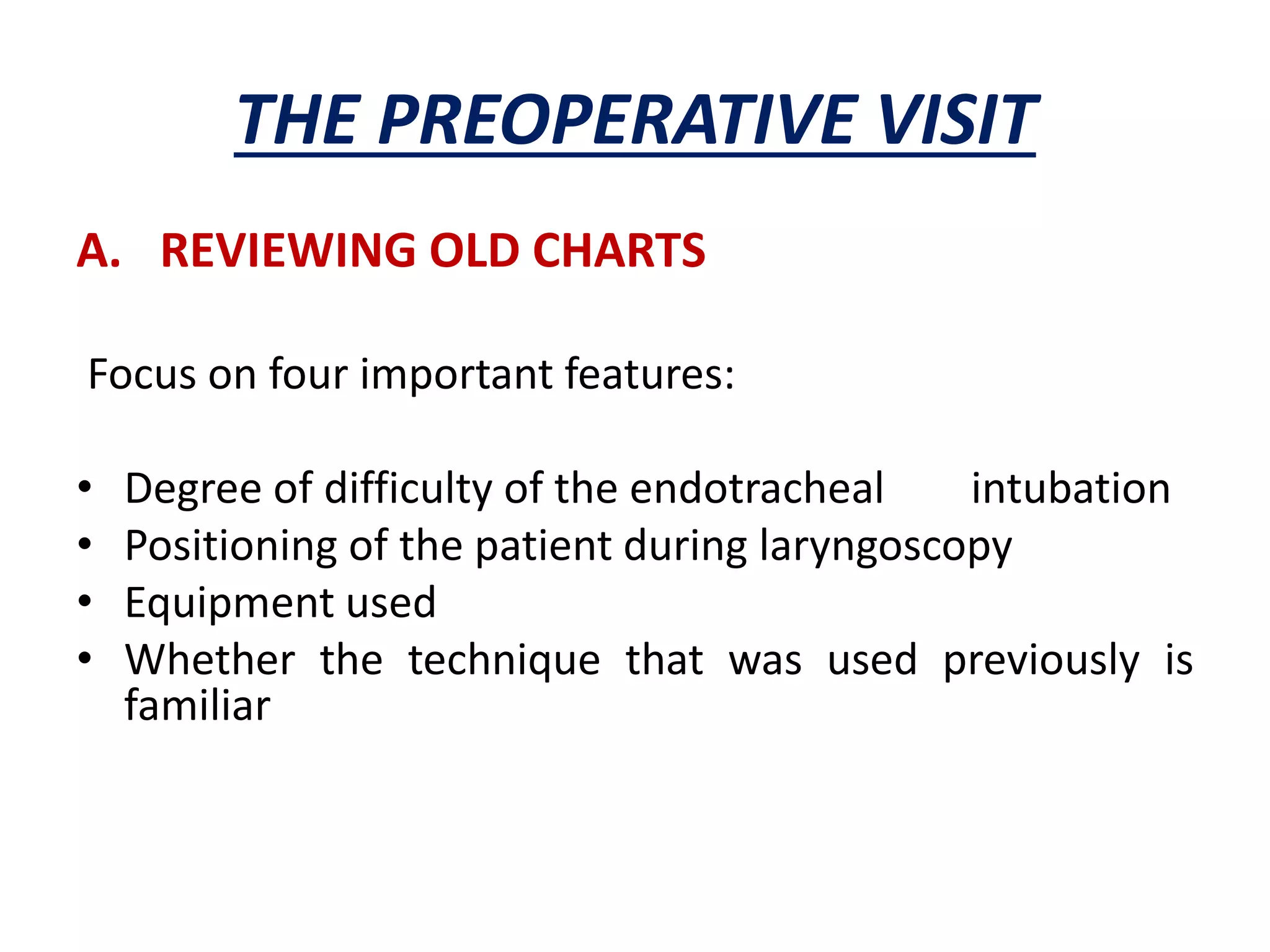
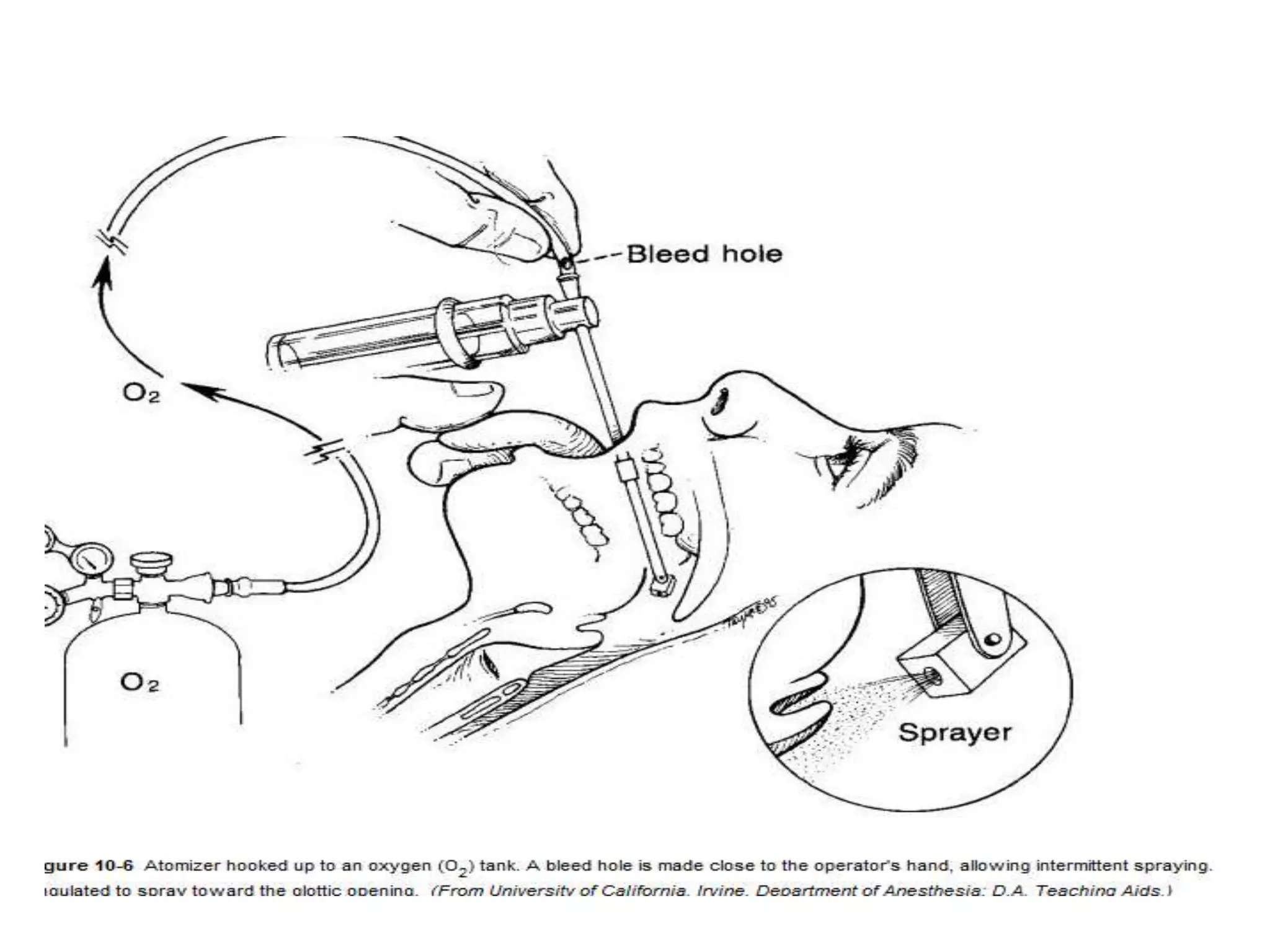
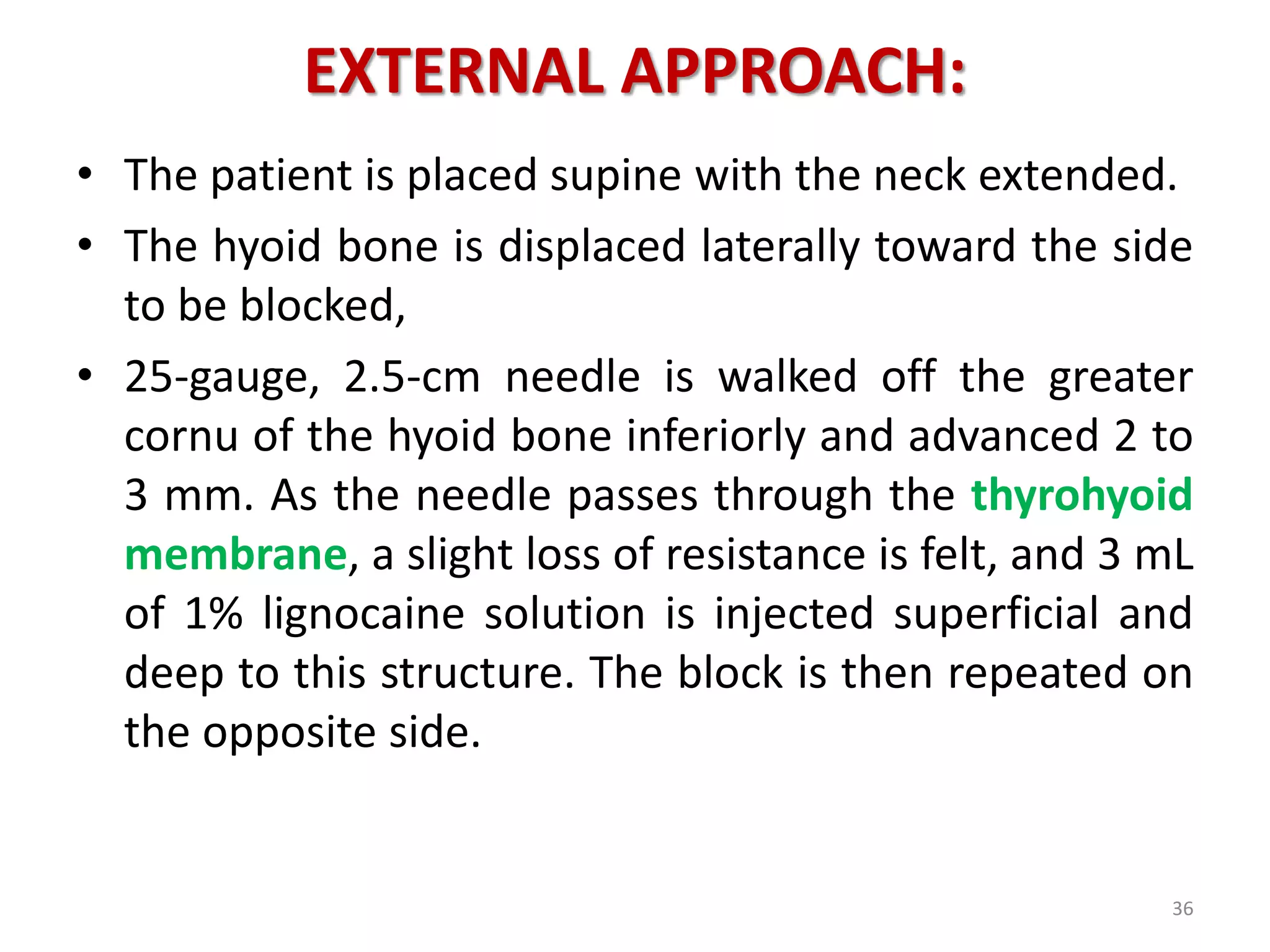
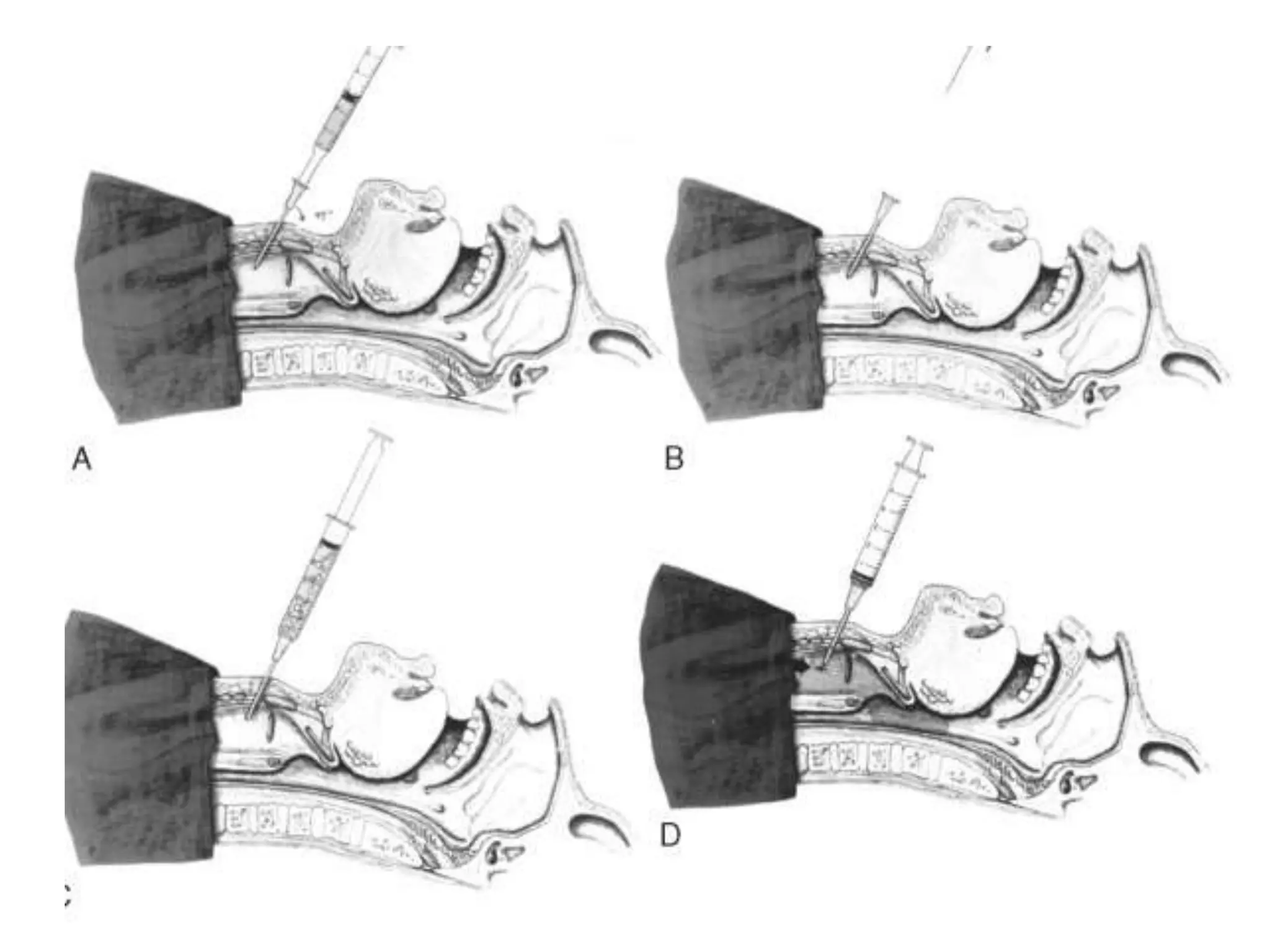
2. Proper preparation includes premedication to alleviate anxiety, dry the airway, and protect against aspiration. Topicalization of the airway with local anesthetics is also important.
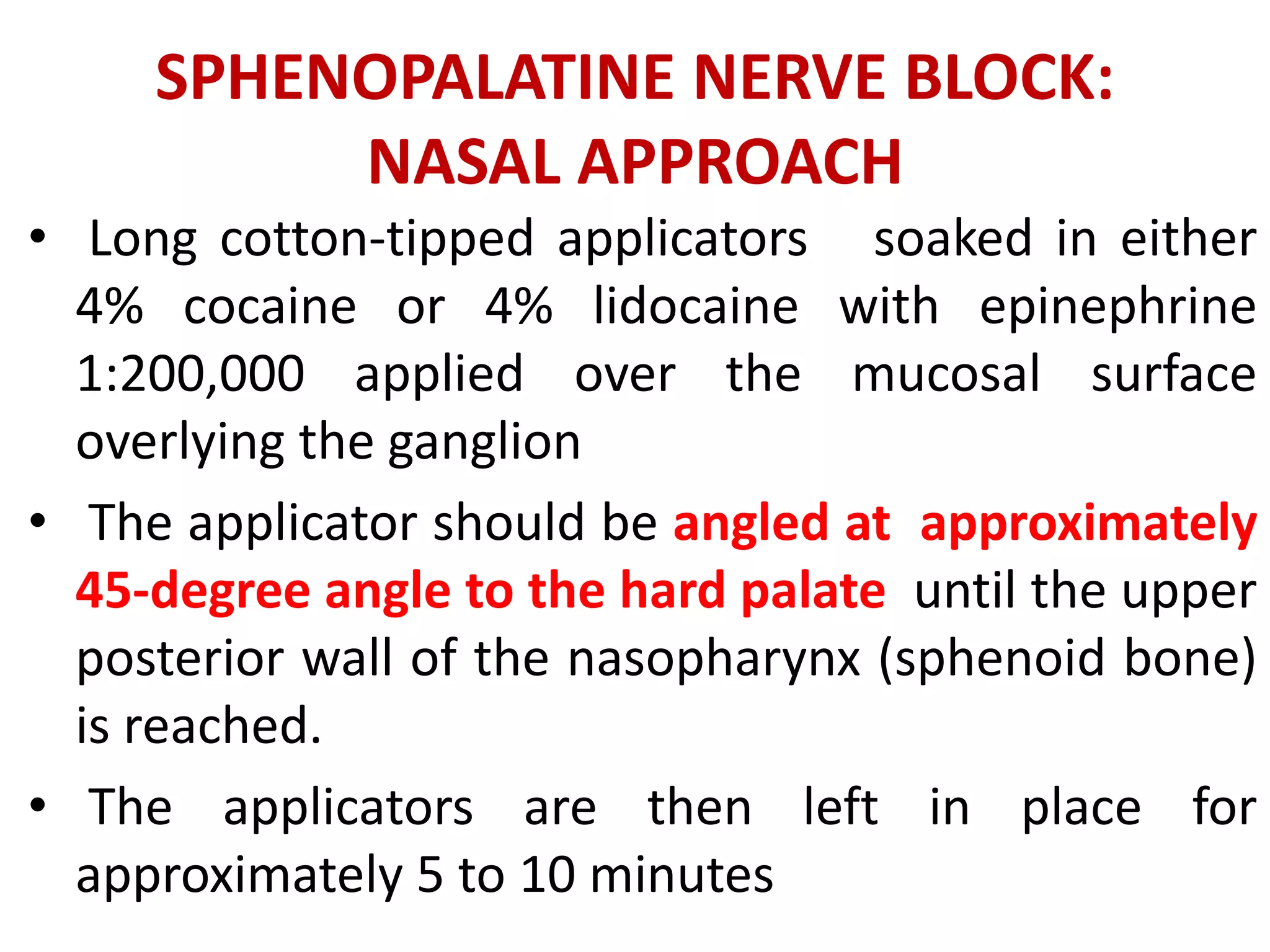
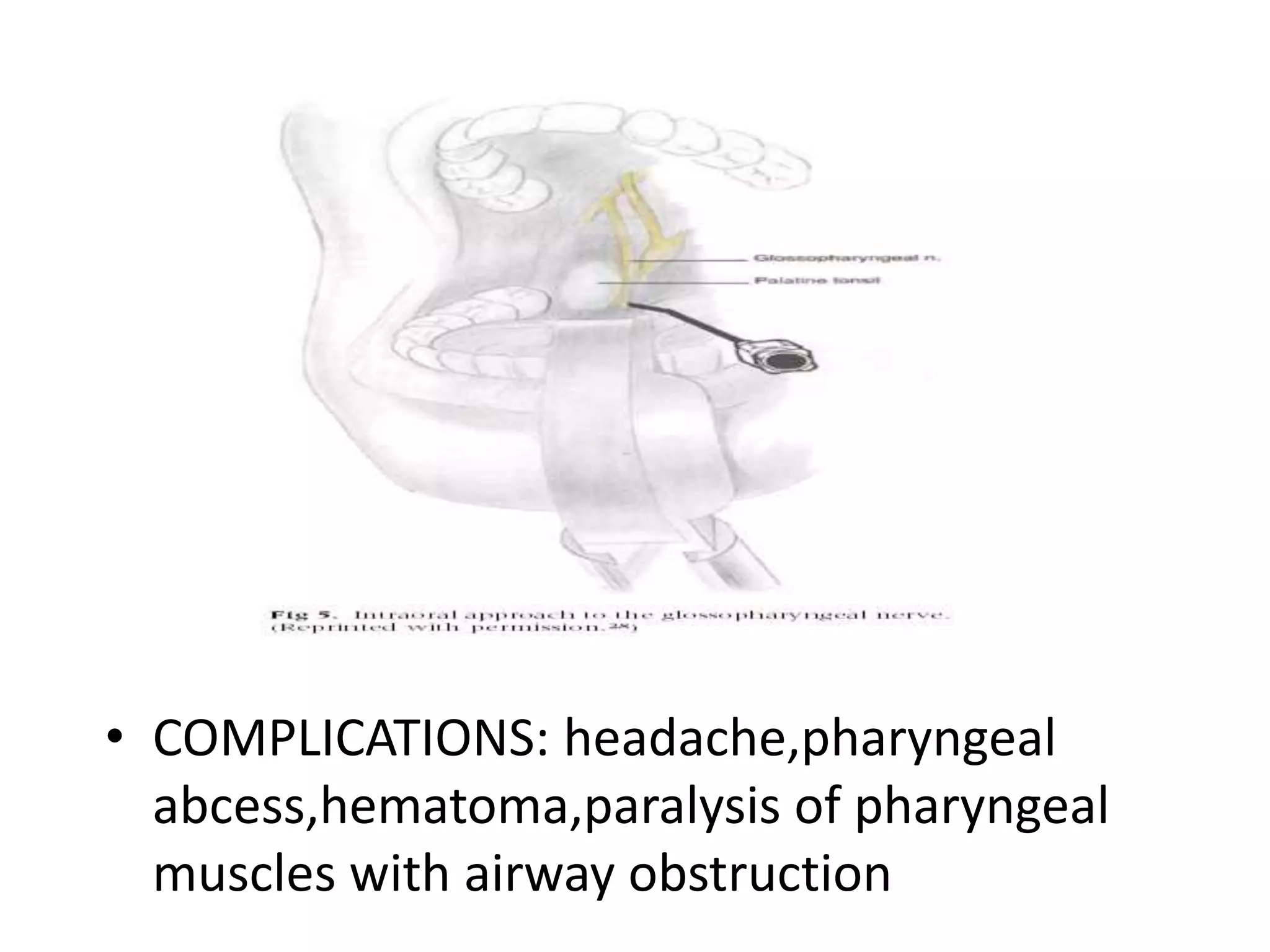
3. Nerve blocks like the sphenopalatine and anterior ethmoidal blocks are used to anesthetize the nasal cavity and nasopharynx during nasal awake intubation.