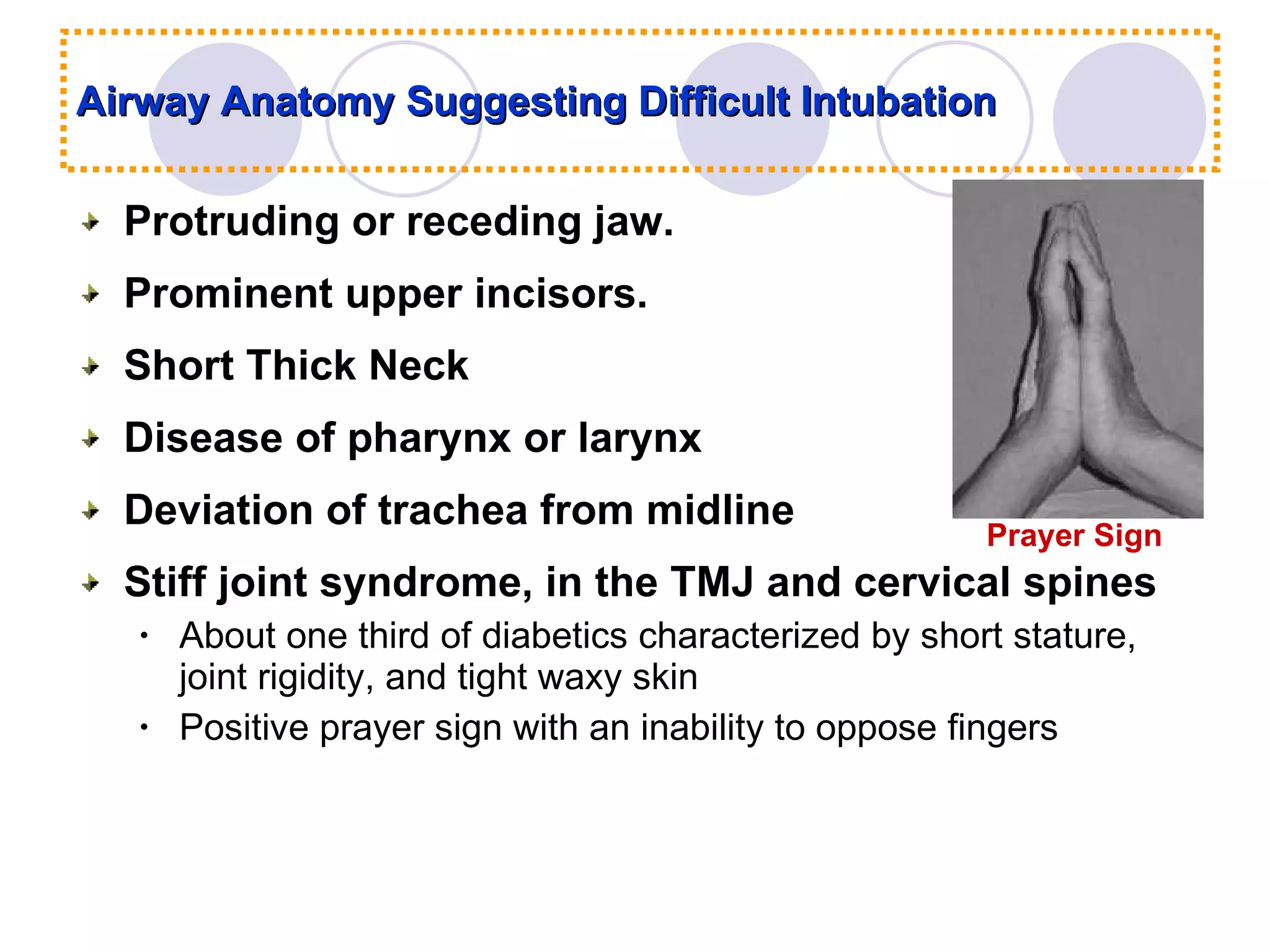
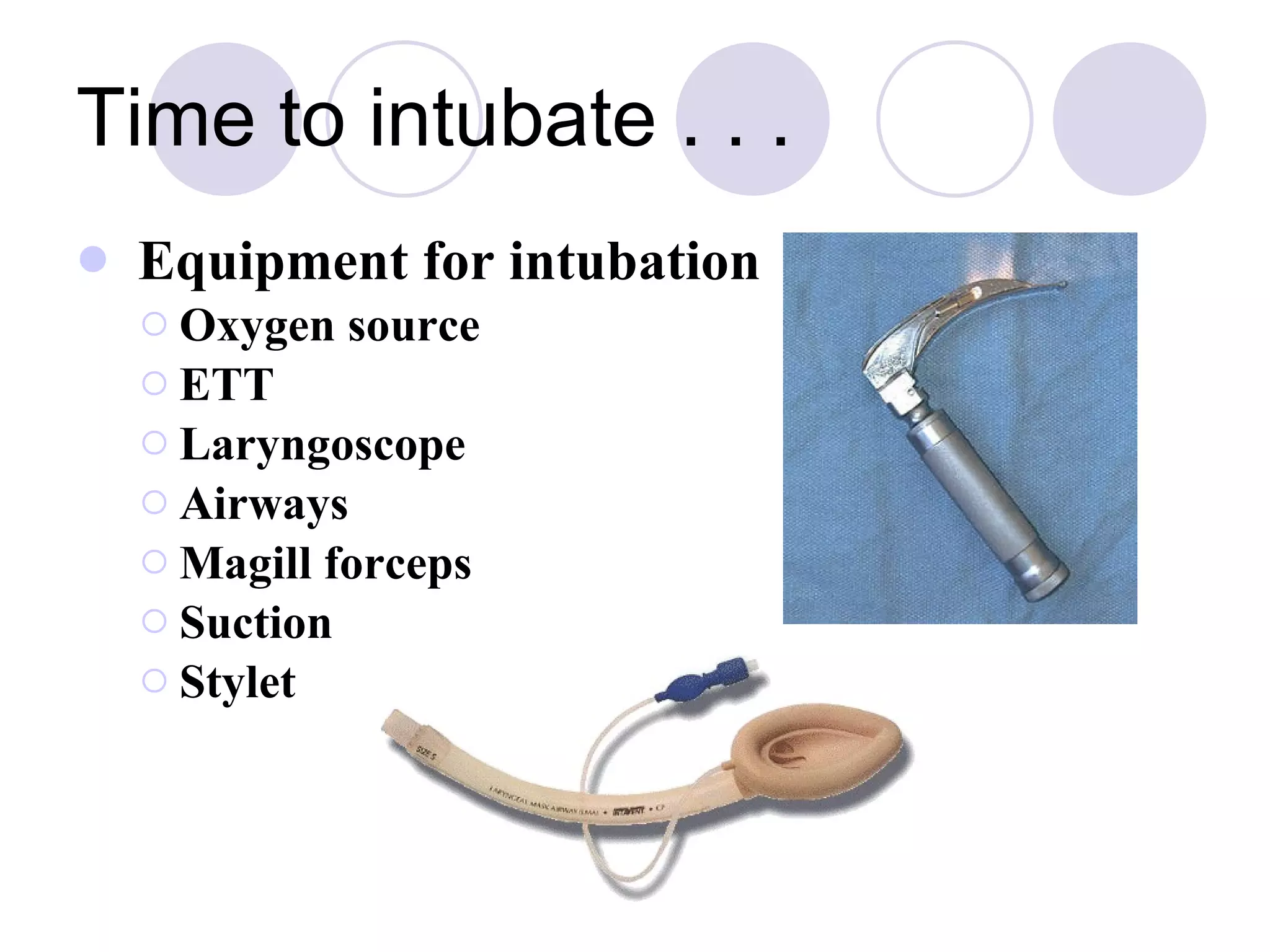
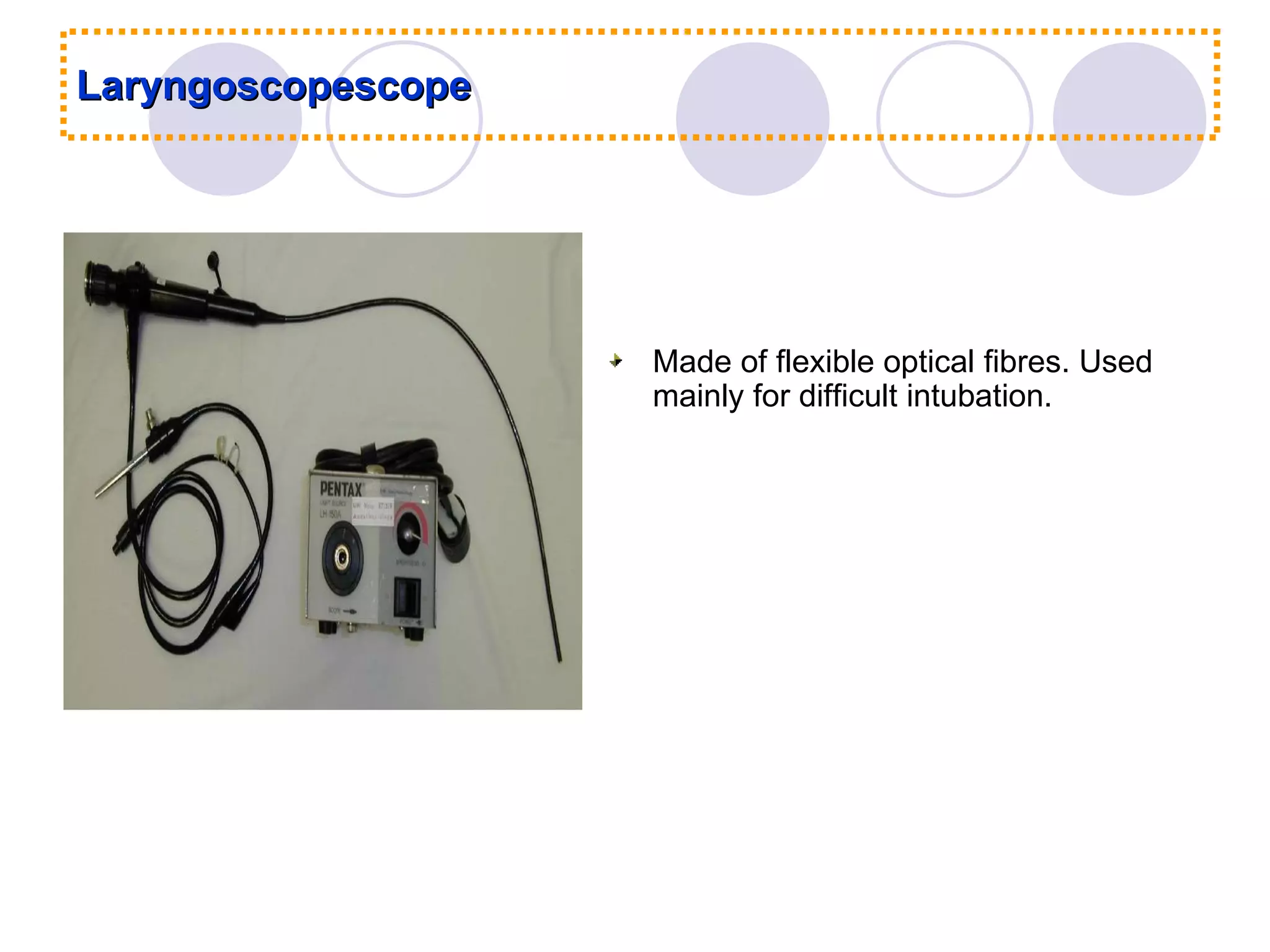
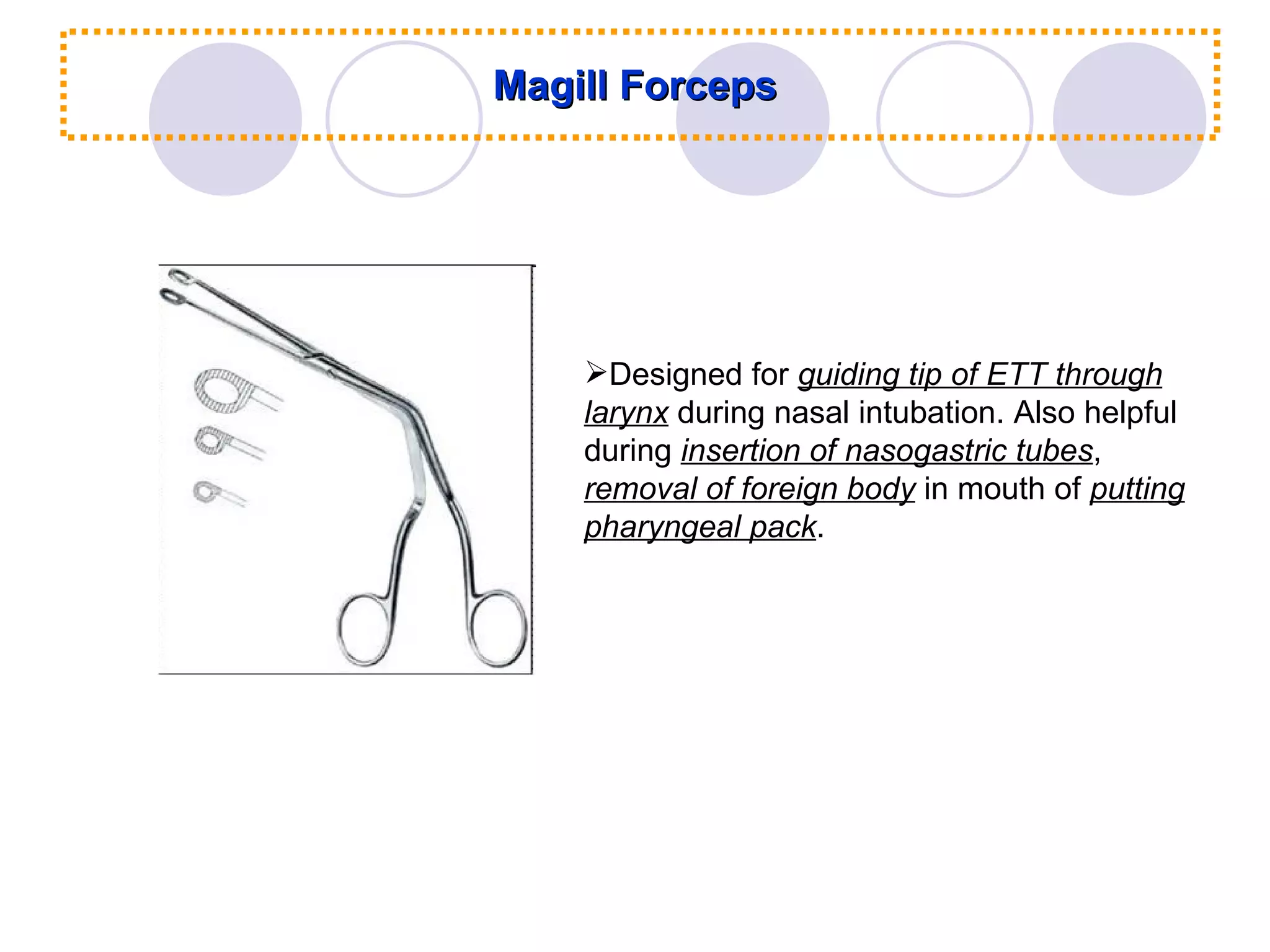
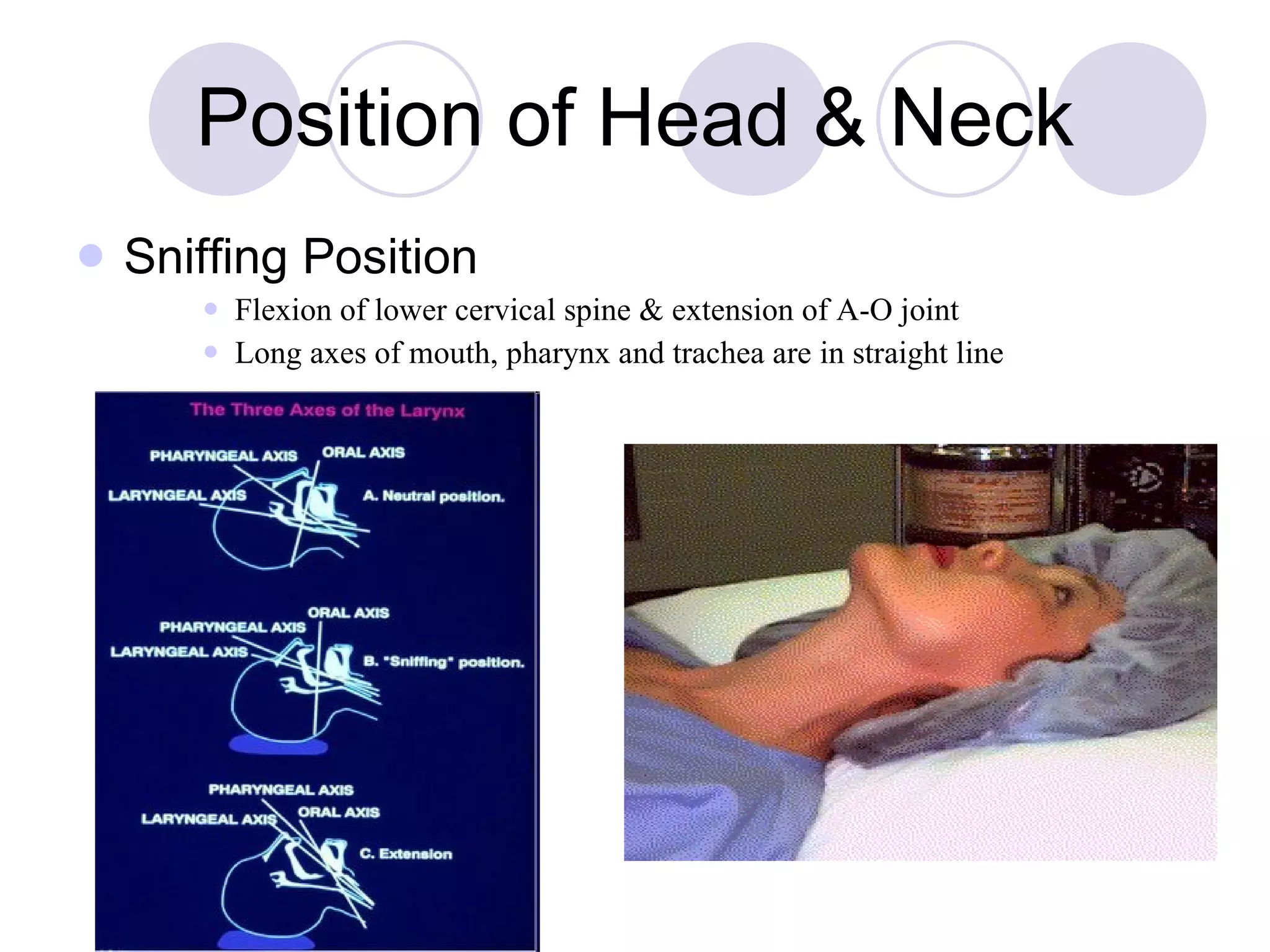
Tracheal intubation involves inserting a tube into the trachea to control ventilation and oxygenation during anesthesia. Various airway devices and techniques are used for intubation. Complications can occur during or after intubation, and careful patient positioning, preparation of equipment, and confirmation of proper tube placement are important to perform intubation safely.