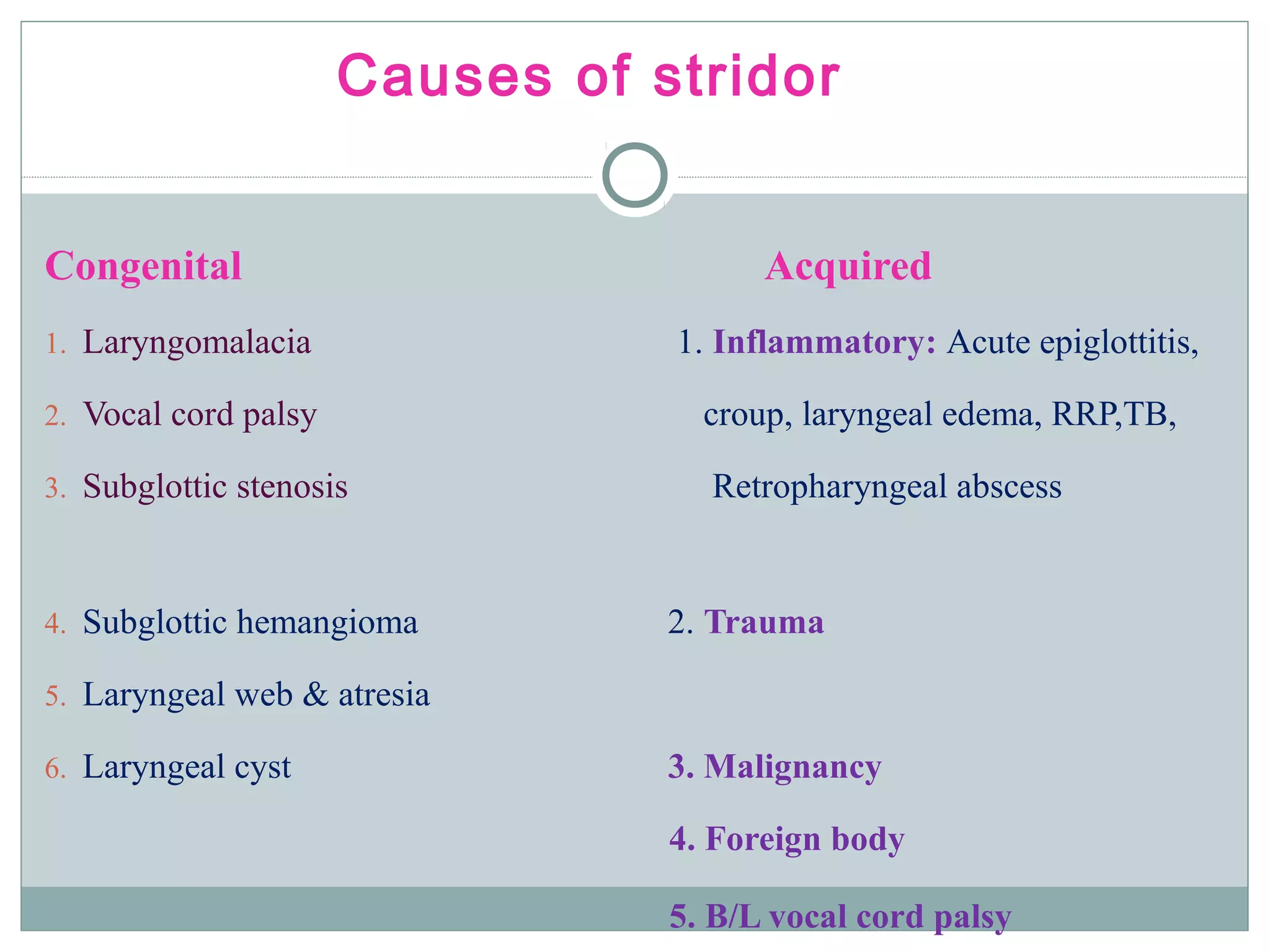
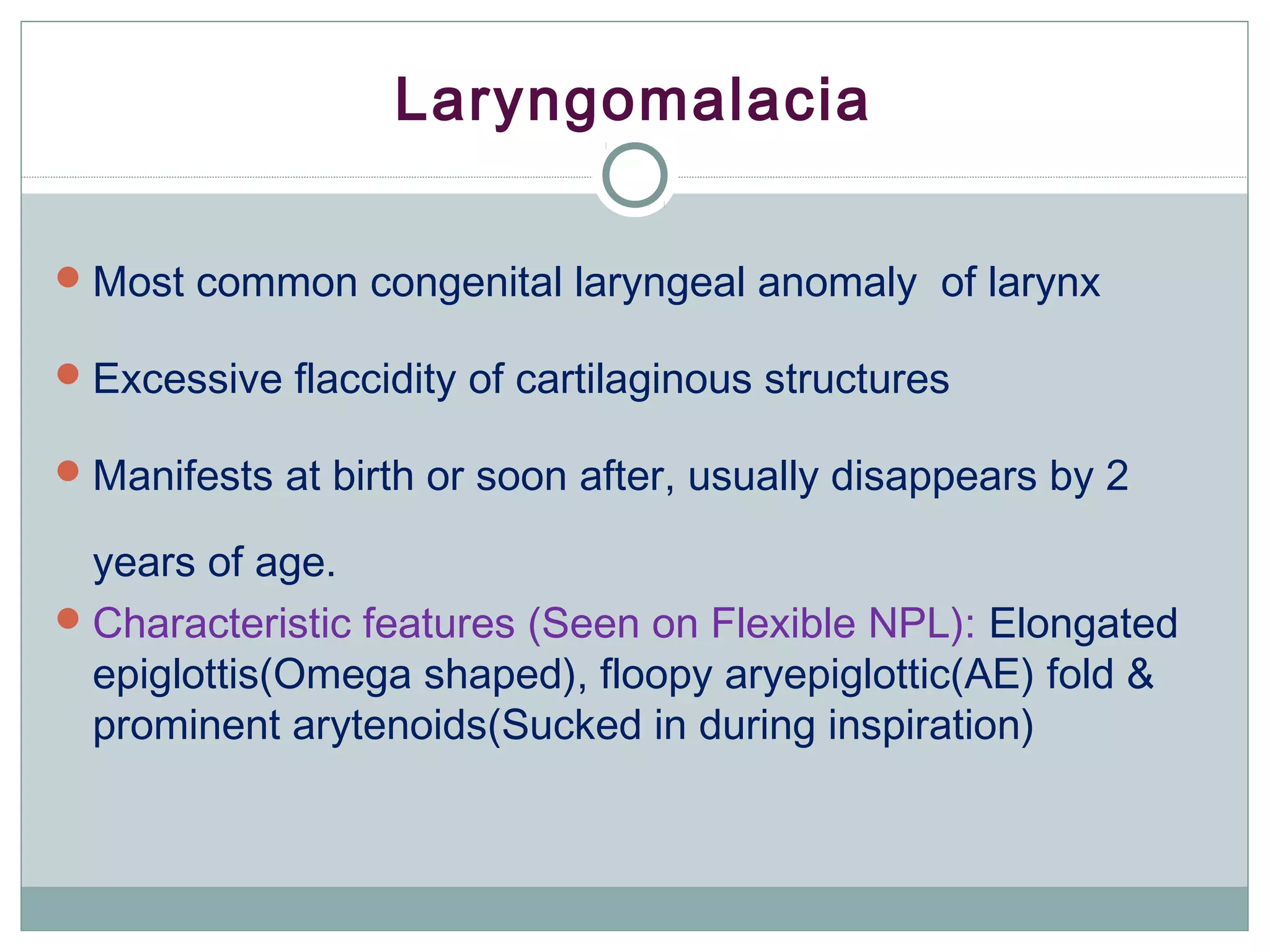
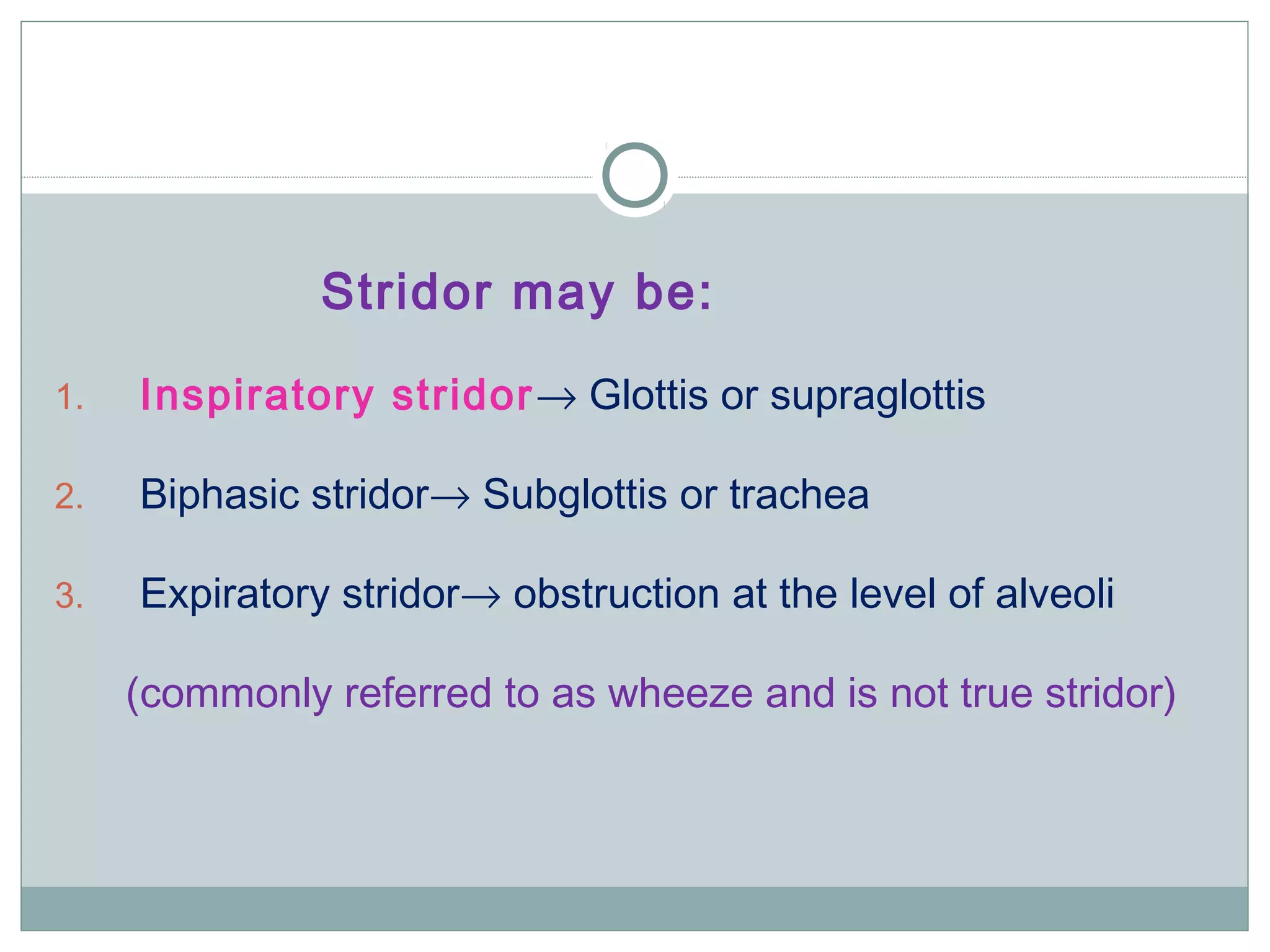
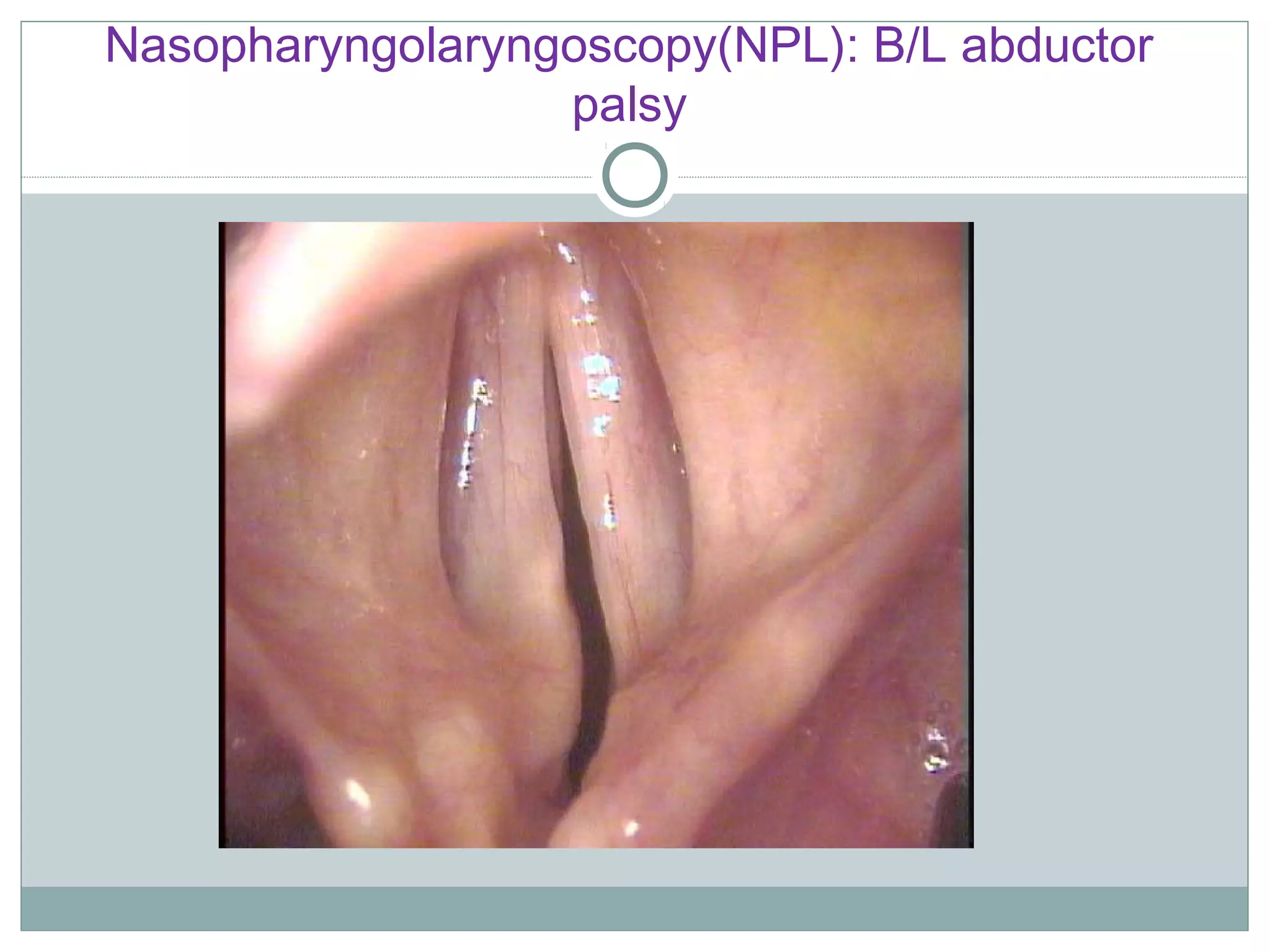
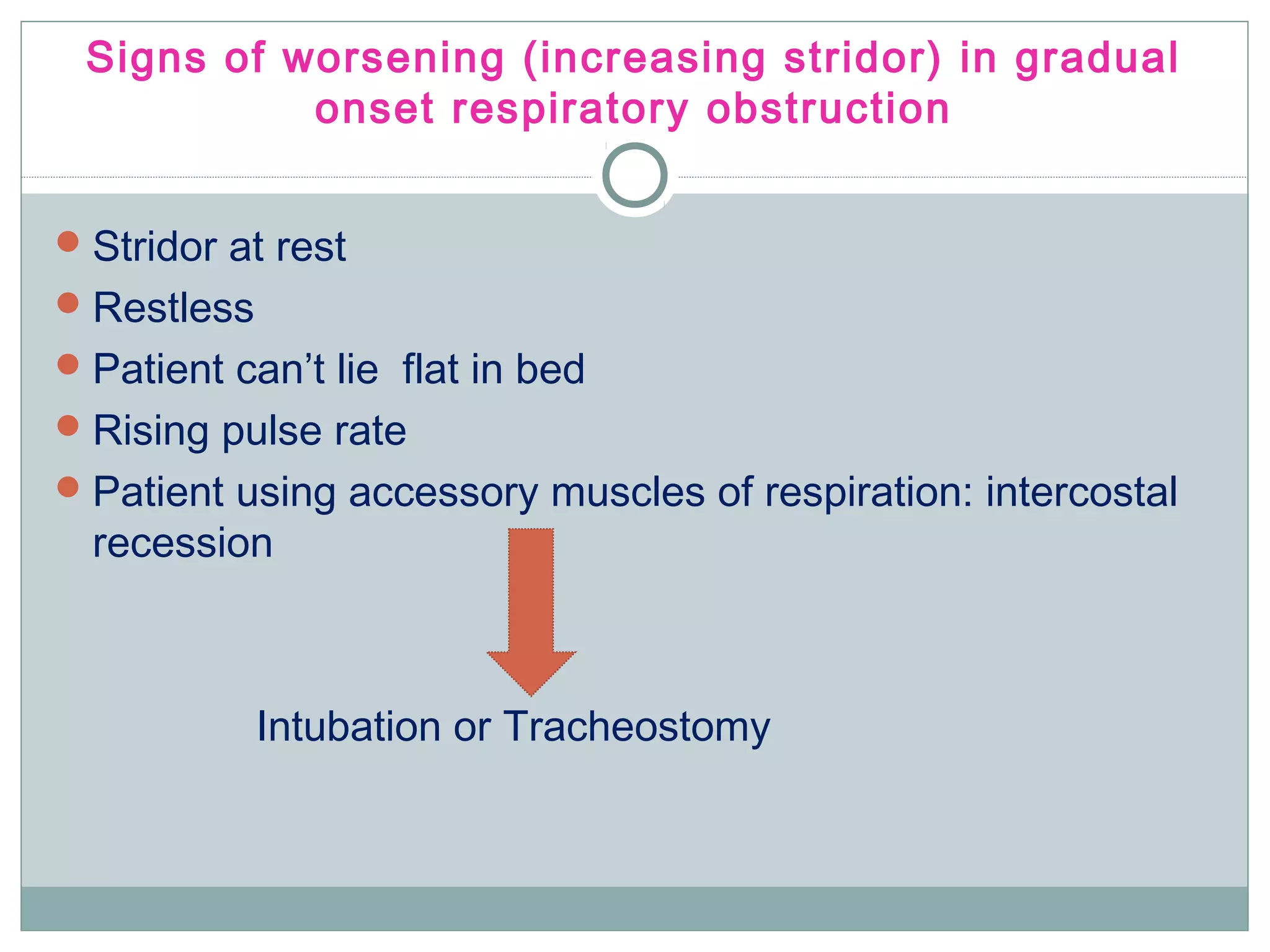
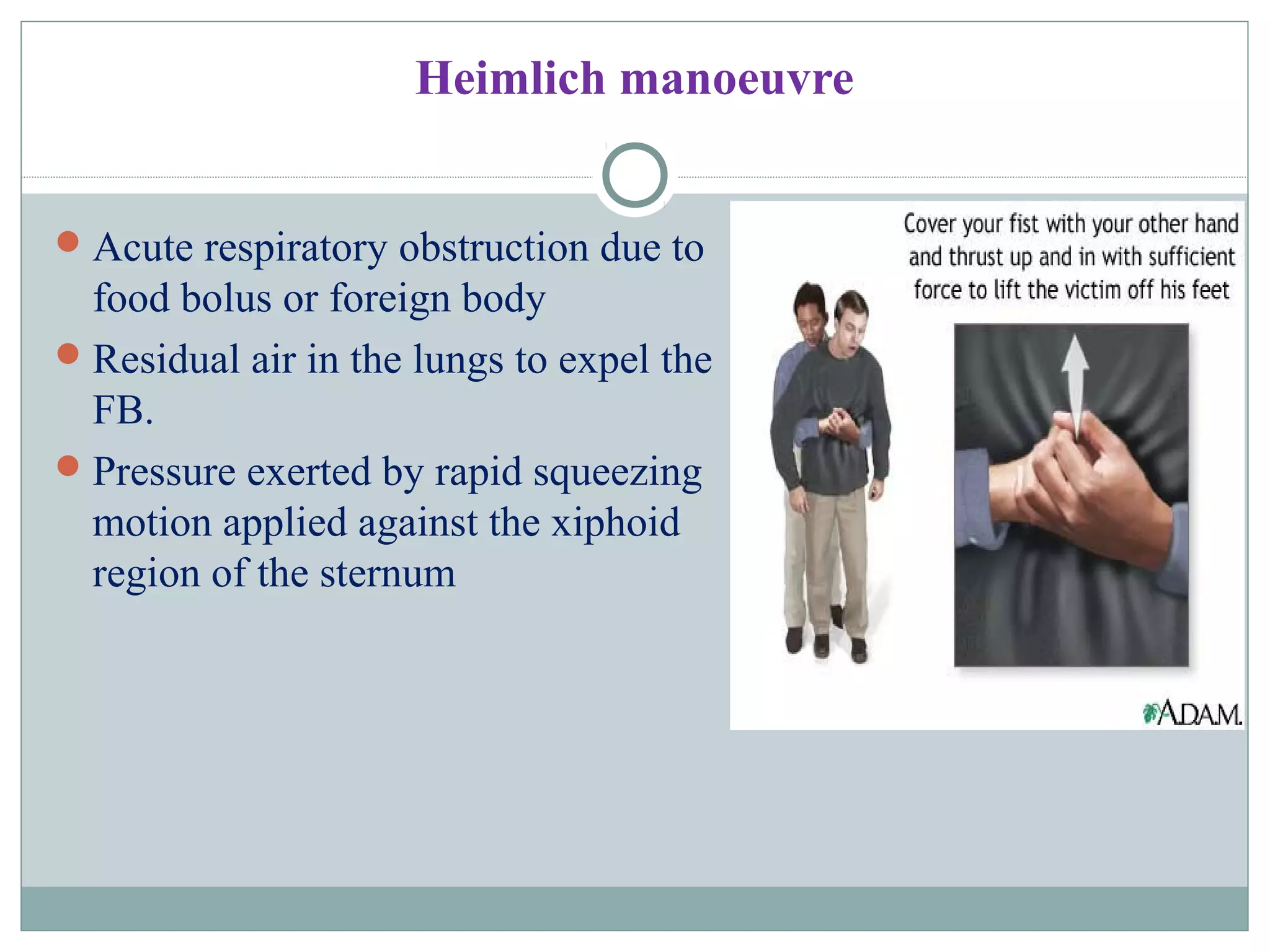
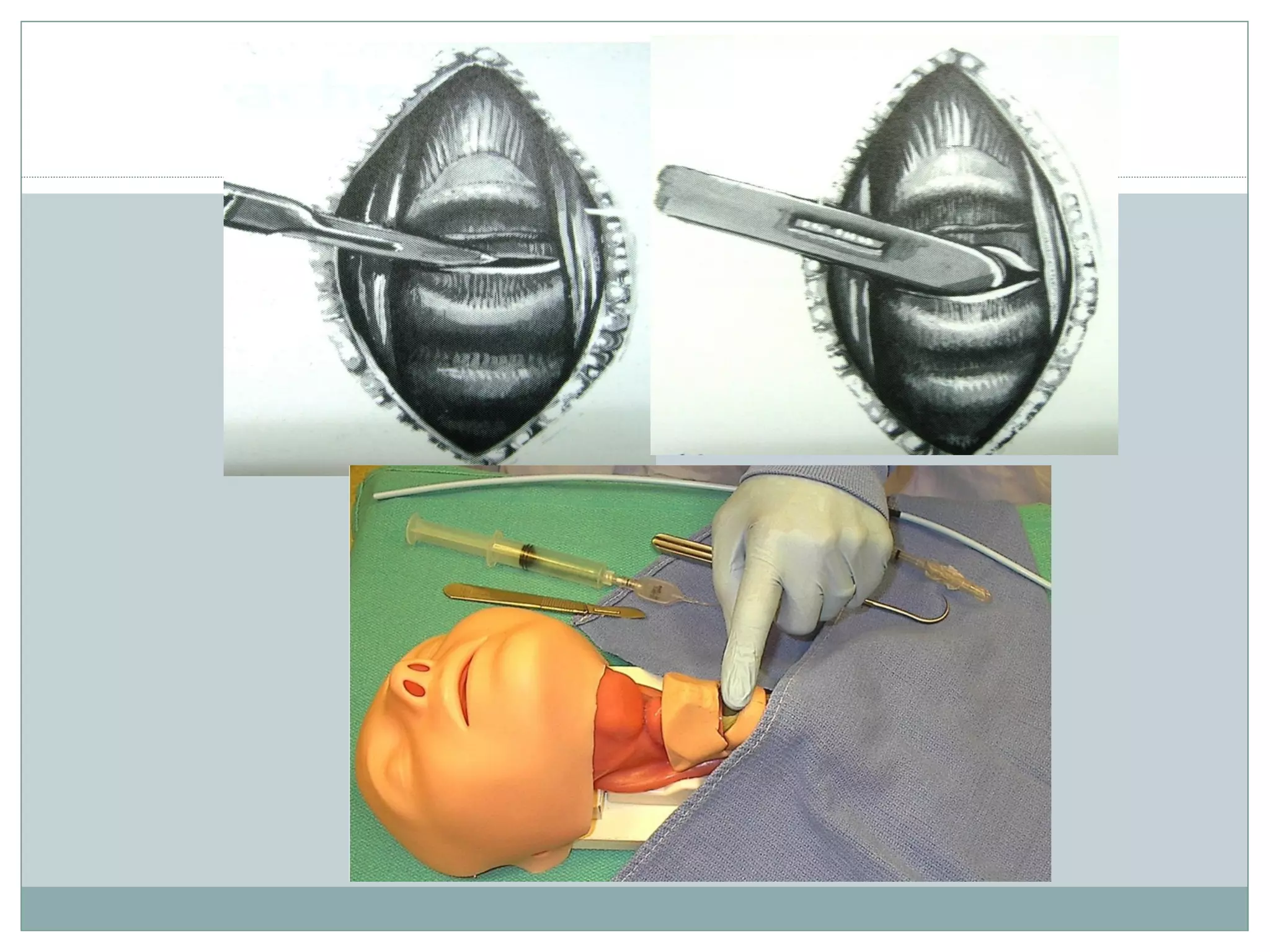
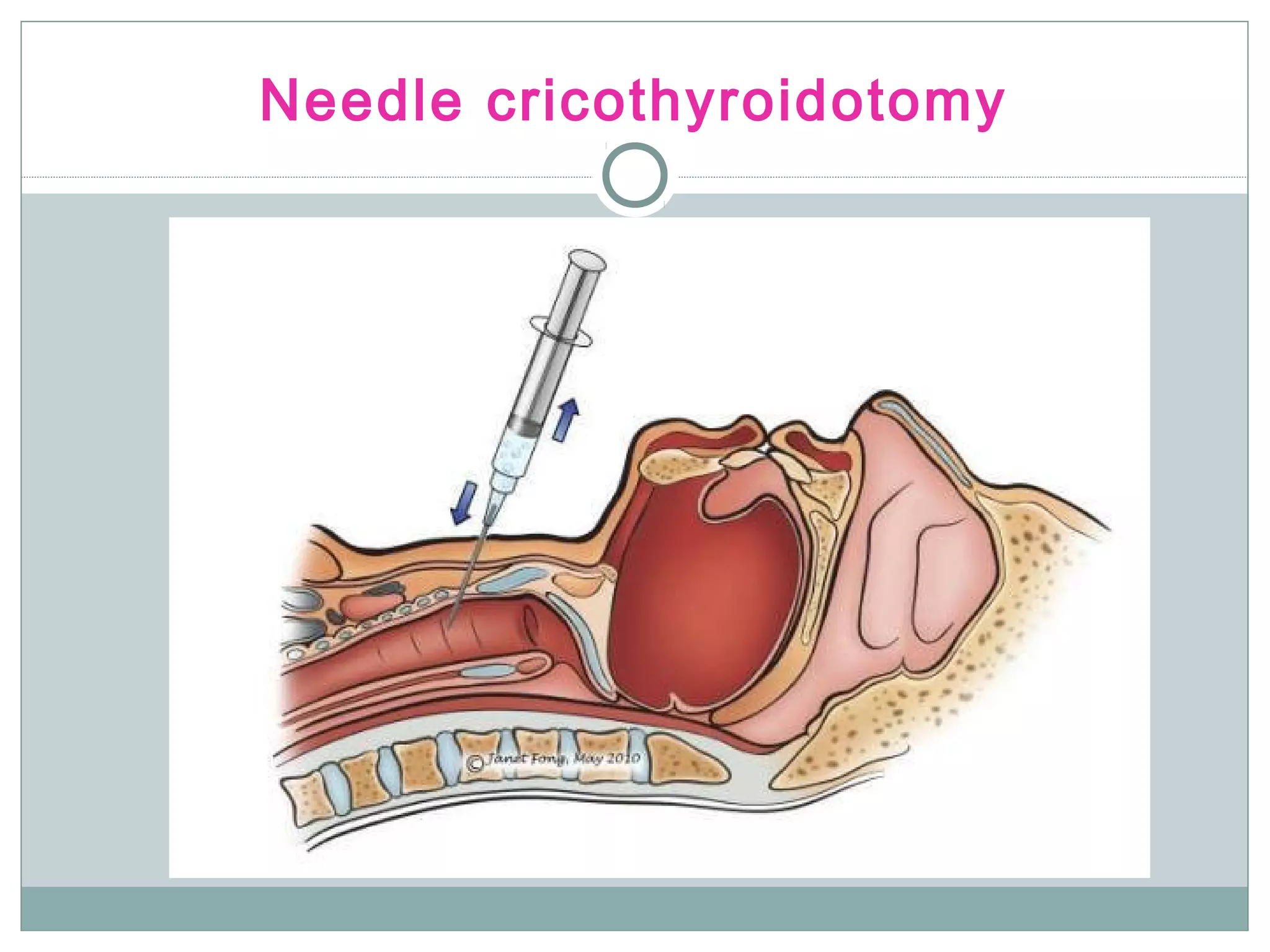
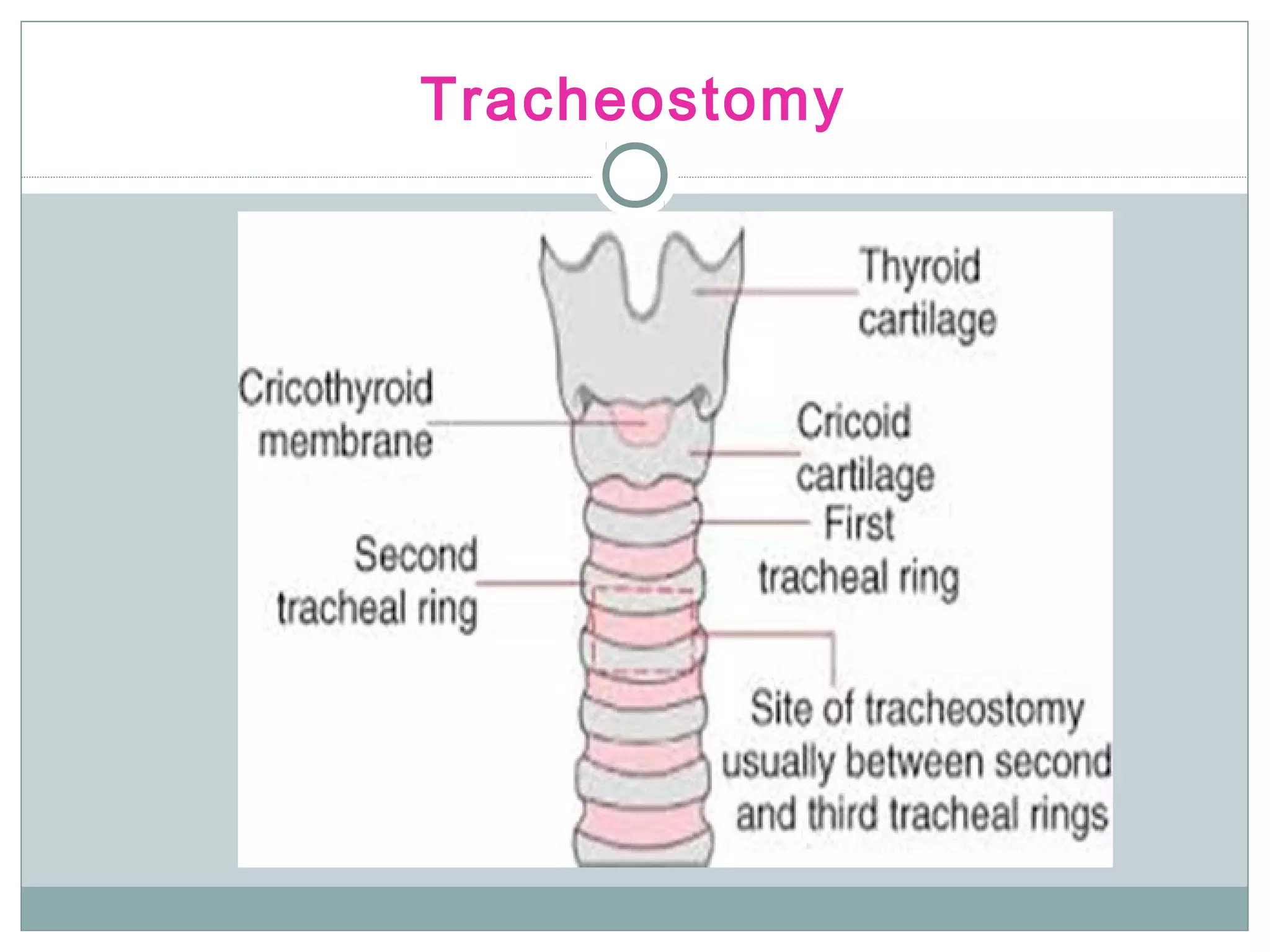
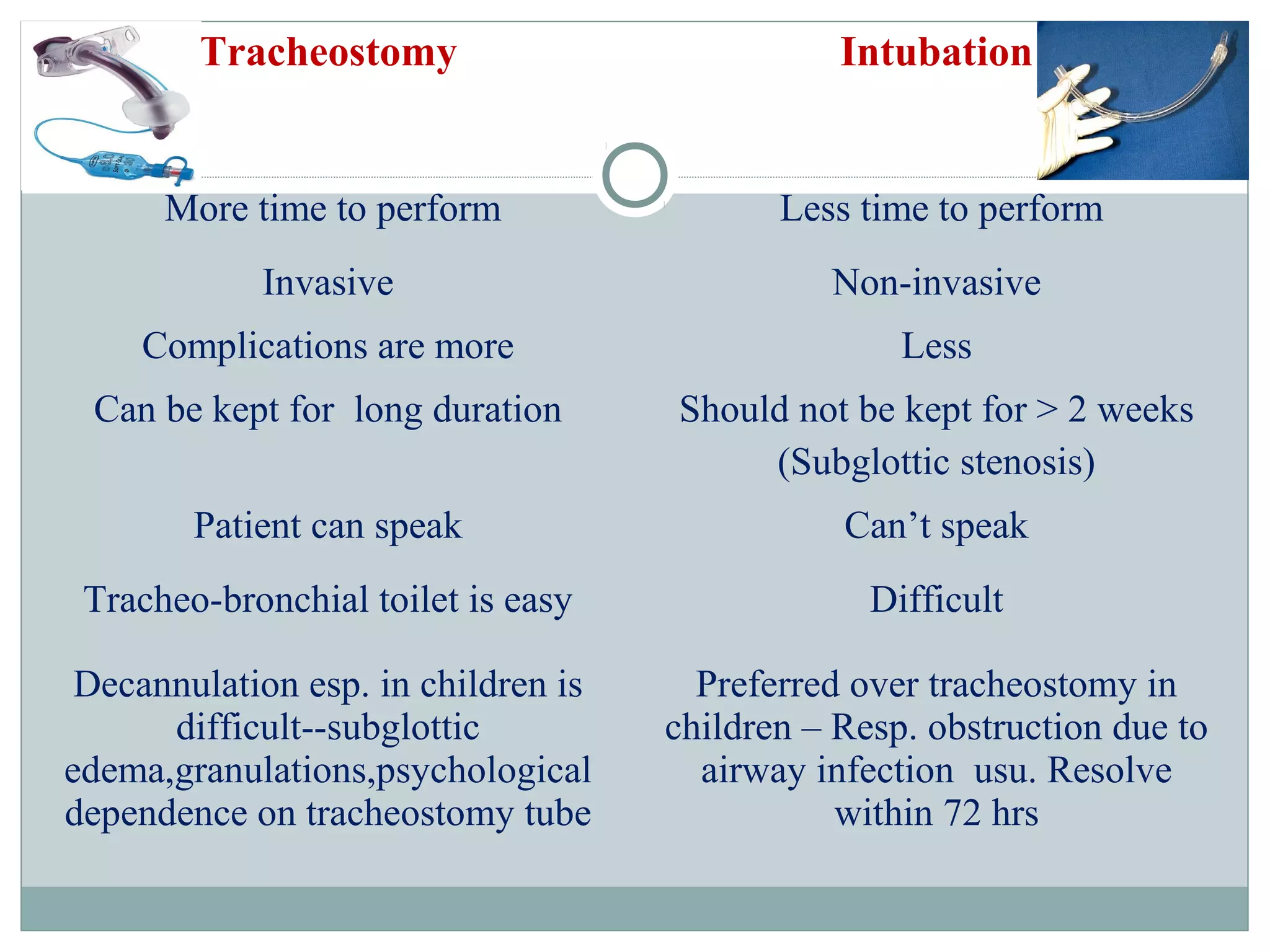
This document discusses various types of noisy breathing and causes of hoarseness and stridor. It describes laryngomalacia as the most common congenital laryngeal anomaly manifesting as inspiratory stridor that is often relieved by prone positioning. For management of obstructed airways, it recommends techniques such as Heimlich maneuver, oropharyngeal/nasal airways, intubation, cricothyroidotomy, tracheostomy based on the level and severity of obstruction. Intubation is preferred over tracheostomy for short term airway issues in children due to easier decannulation and lower risk of subglottic stenosis.