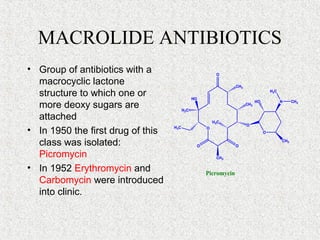
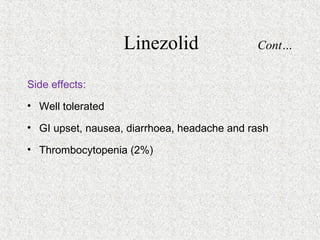
This document discusses several classes of antibiotics including macrolides, clindamycin, vancomycin, linezolid, and polypeptide antibiotics. It provides details on the mechanism of action, pharmacokinetics, resistance, uses, and side effects of erythromycin, clarithromycin, azithromycin, roxithromycin, clindamycin, vancomycin, linezolid, polymyxin B, colistin, and bacitracin.