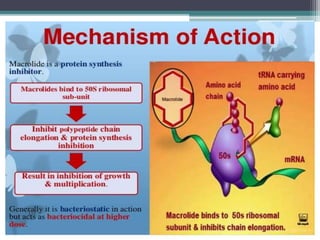
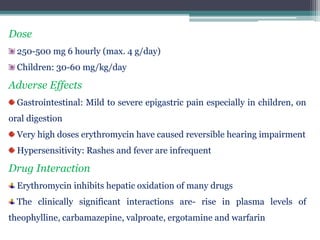
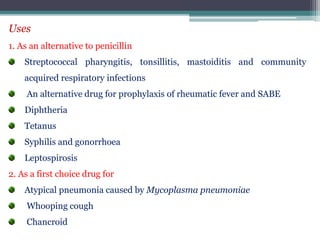
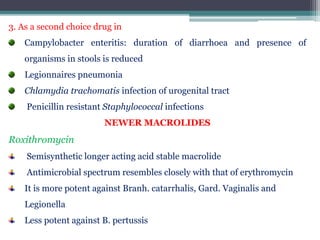
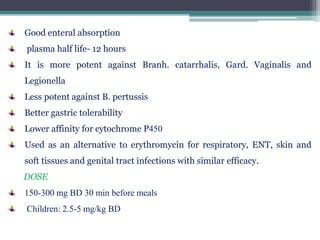
Macrolide antibiotics contain a macrocyclic lactone ring with attached sugars. Erythromycin, the first macrolide discovered in the 1950s, is produced by Streptomyces erythreus. Newer macrolides like roxithromycin and clarithromycin have improved properties compared to erythromycin such as better absorption and tolerability. Macrolides bind to the 50s subunit of the bacterial ribosome, inhibiting protein synthesis and thus exhibiting bacteriostatic and sometimes bactericidal activity. They are effective against many gram-positive bacteria and atypical pathogens. Resistance can develop via efflux pumps or methylation of the ribosomal binding site.