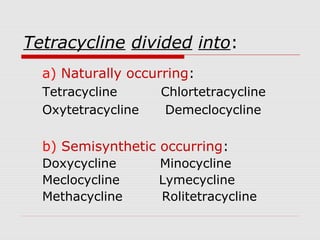
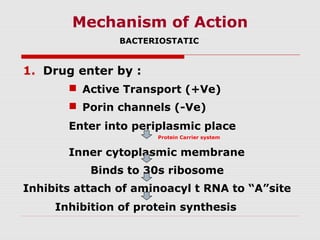
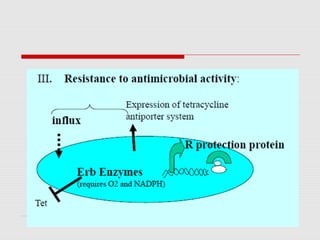
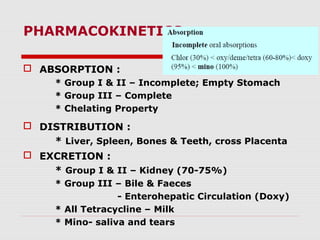
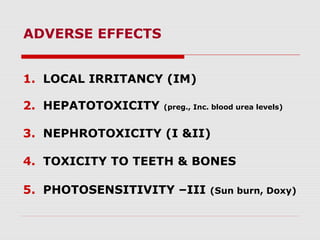
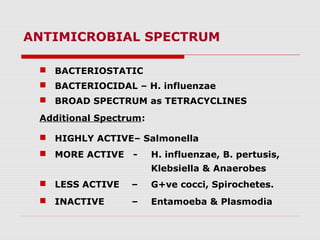
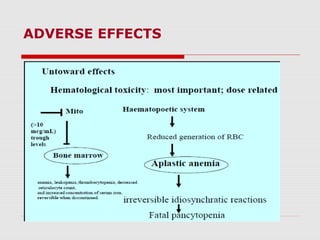
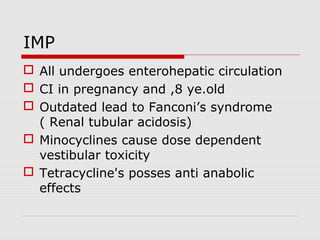
This document summarizes broad spectrum antibiotics tetracyclines and chloramphenicol. It describes the classification, mechanisms of action, antimicrobial spectrum, resistance, pharmacokinetics, adverse effects and therapeutic uses of tetracyclines. It also summarizes the mechanism of action, antimicrobial spectrum, resistance, pharmacokinetics, adverse effects and therapeutic uses of chloramphenicol. Both antibiotics are bacteriostatic, have broad spectra, can cause bone marrow toxicity and are enterohepatically circulated.