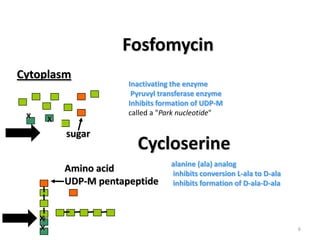
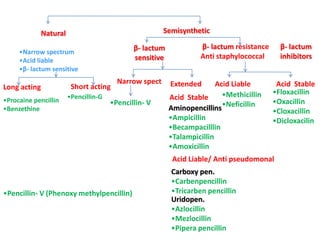
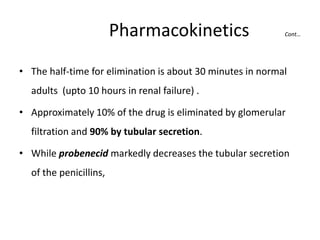
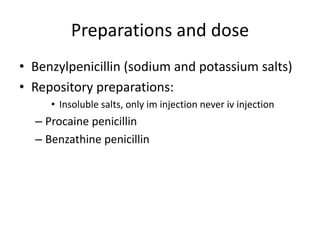
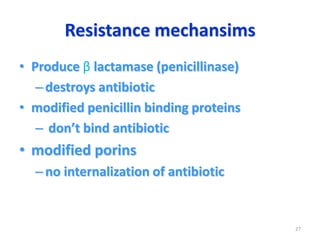
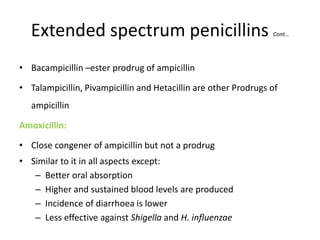
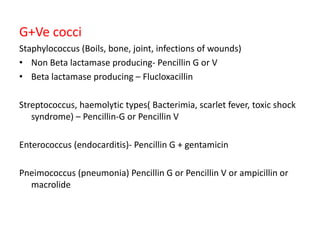
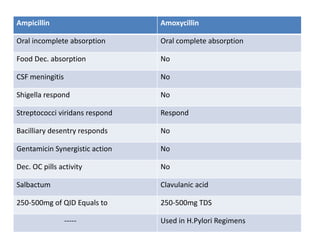
This document discusses various antibiotics that act on the bacterial cell wall. It begins by describing the structure and function of the bacterial cell wall and how antibiotics can disrupt it. It then lists several common antibiotics that target the cell wall, including penicillin, cephalosporins, cycloserine, bacitracin, and vancomycin. It provides details on the source and therapeutic uses of each. The remainder of the document goes into further depth about the mechanisms of action and effects of beta-lactam antibiotics like penicillin, focusing on how they inhibit cell wall synthesis and cross-linking. It describes the structures, spectra, uses and side effects of various penicillin derivatives in detail.