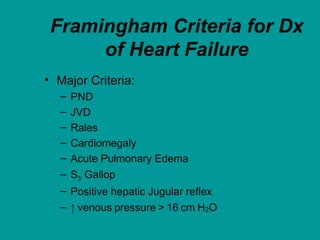
This document provides an overview of heart failure, including its definition, etiology, pathophysiology, symptoms, diagnosis, and treatment. Some key points:
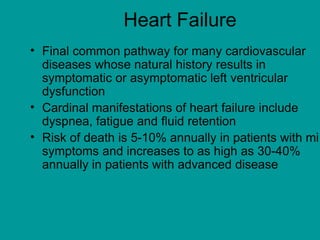
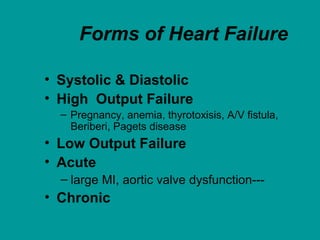
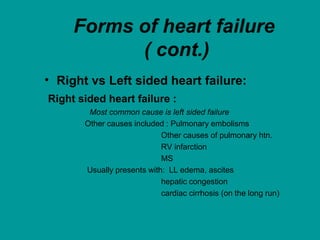
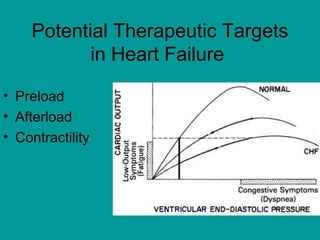
- Heart failure occurs when the heart cannot pump enough blood to meet the body's needs. It is commonly called congestive heart failure due to prominent symptoms of increased venous pressure.
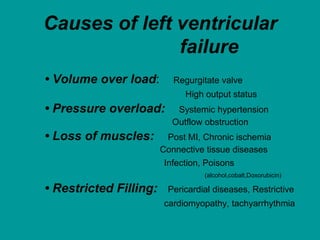
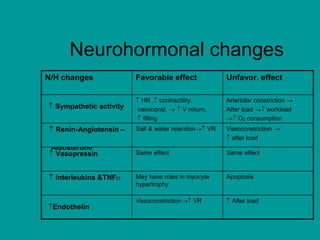
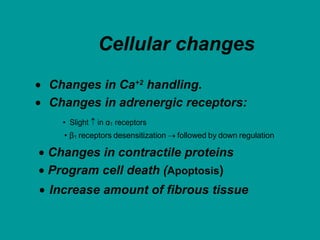
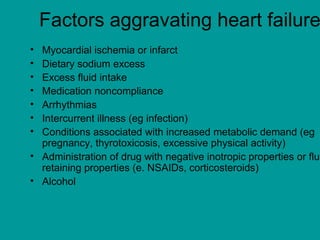
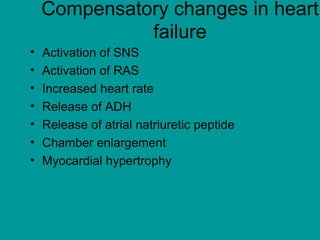
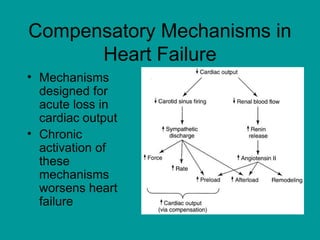
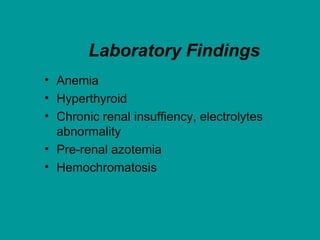
- Common causes include coronary artery disease, hypertension, valvular heart disease, and cardiomyopathy. The final pathway involves neurohormonal activation and changes in cardiac structure and function.
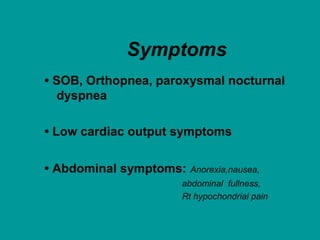
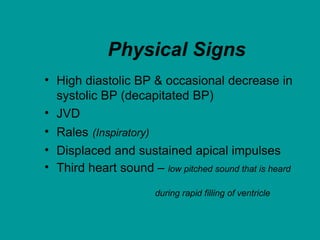
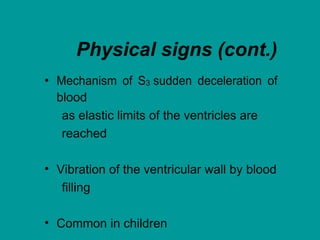
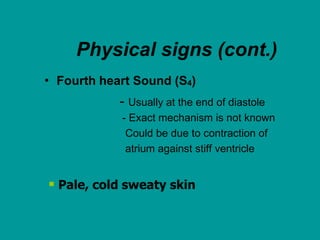
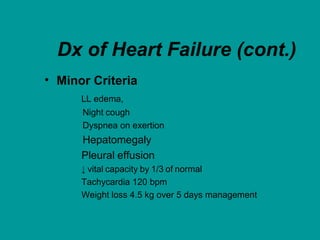
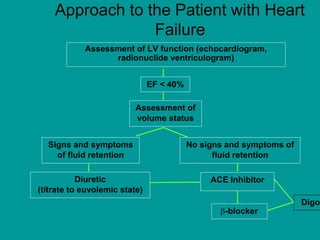
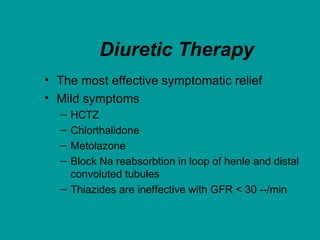
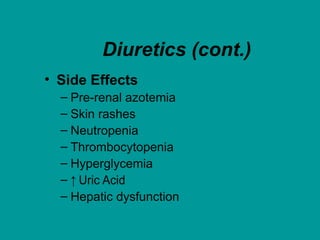
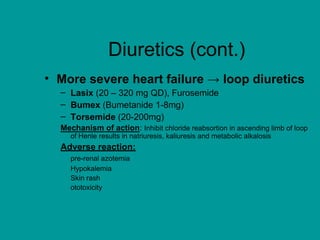
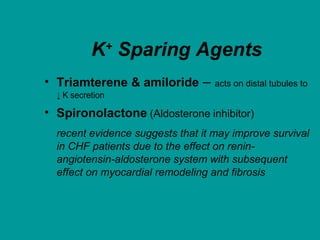
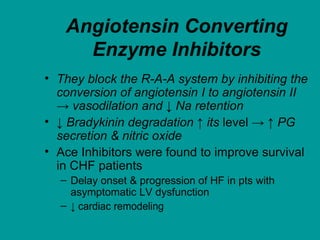
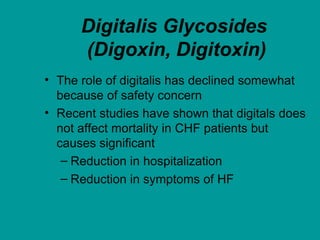
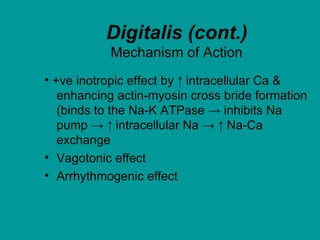
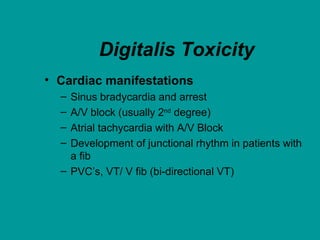
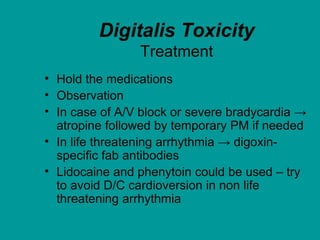
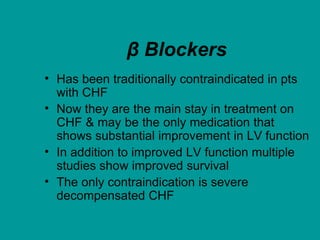
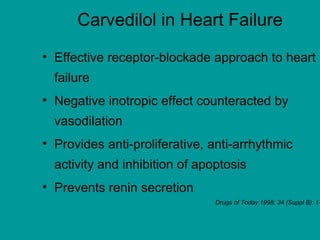
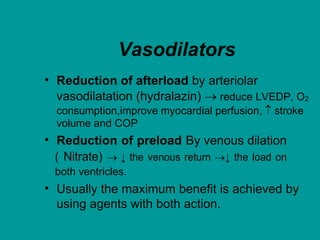
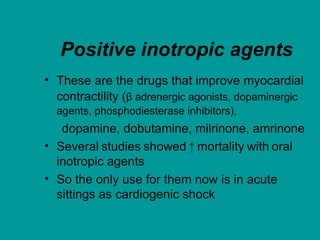
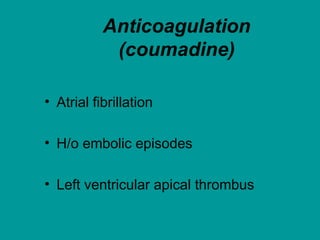
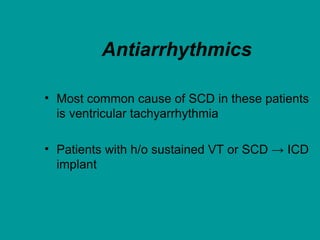
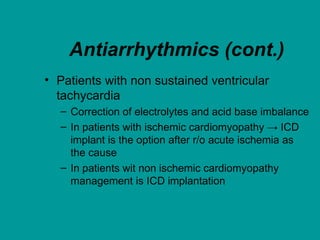
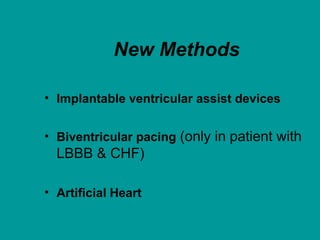
- Symptoms include shortness of breath, fatigue, and fluid retention. Treatment focuses on correcting reversible causes, restricting sodium/fluid intake, and medications like diuretics, ACE