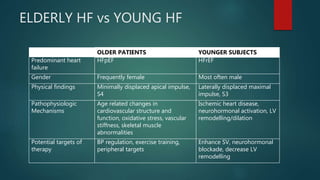
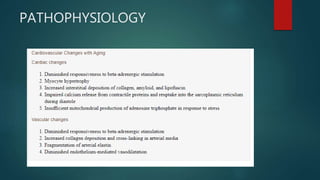
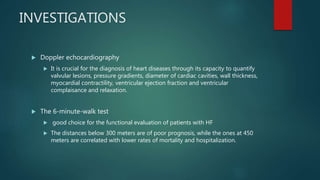
Heart failure is a common condition in elderly patients, affecting over 80% of all heart failure patients aged 65 and older. It is often difficult to diagnose and manage heart failure in elderly patients due to multiple comorbidities and polypharmacy. While the symptoms of heart failure are similar between elderly and younger patients, the causes and treatments may differ, with conditions like hypertension and coronary artery disease being more common causes in elderly patients. Echocardiography is important for determining left ventricular ejection fraction to guide use of treatments like ACE inhibitors, beta-blockers, diuretics and digitalis, which can help manage symptoms and prolong life for elderly heart failure patients.