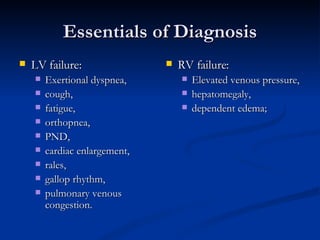
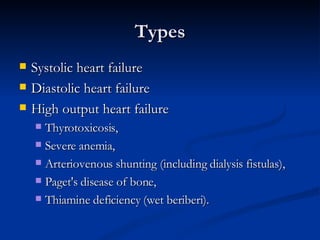
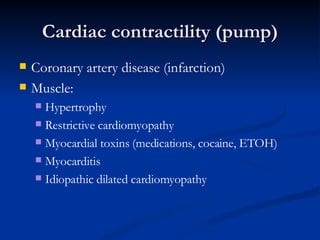
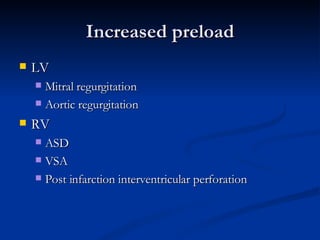
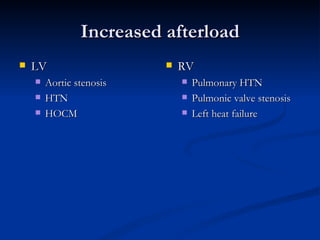
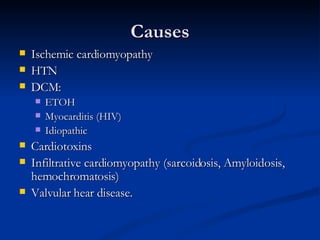
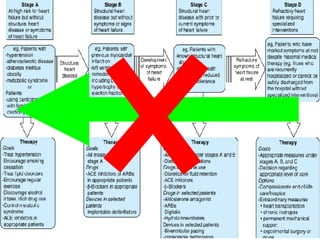
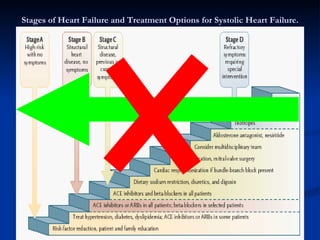
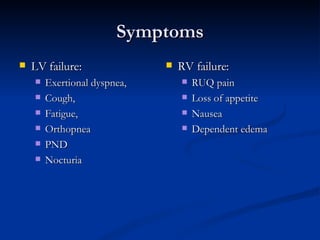
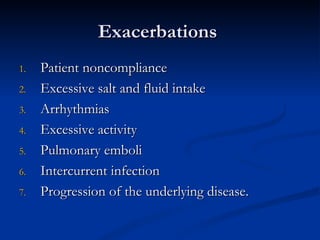
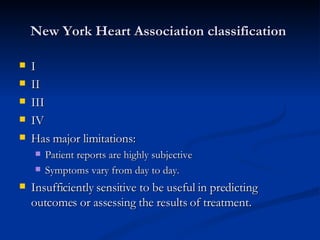
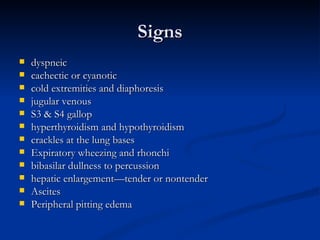
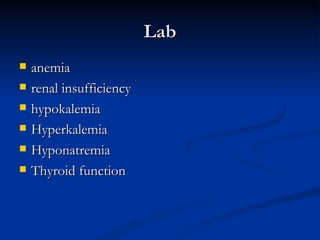
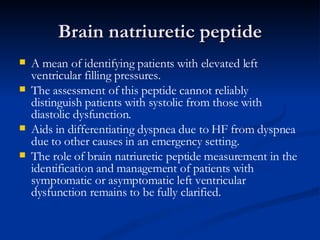
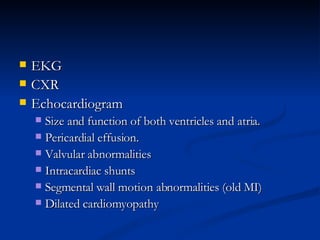
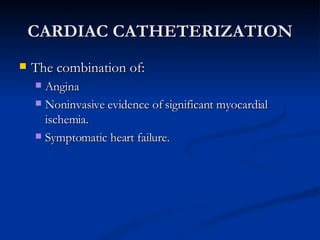
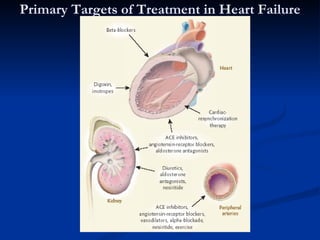
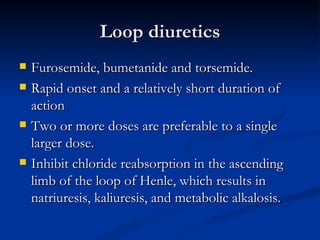
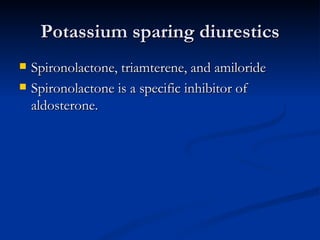
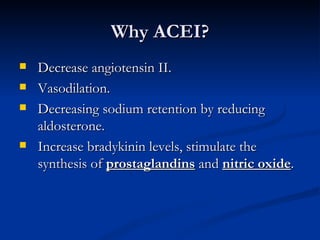
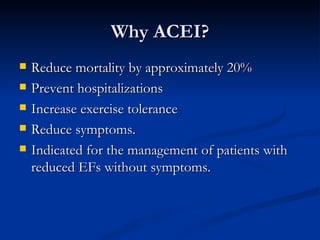
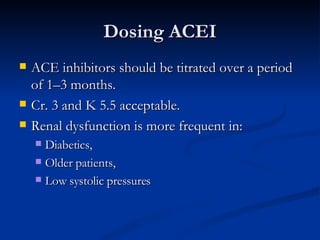
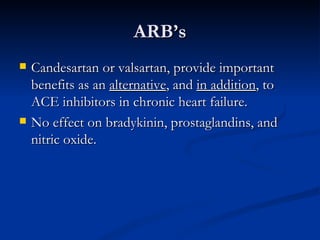
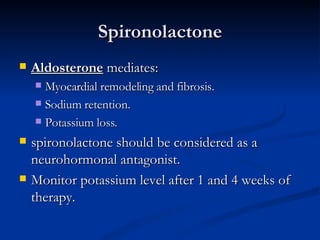
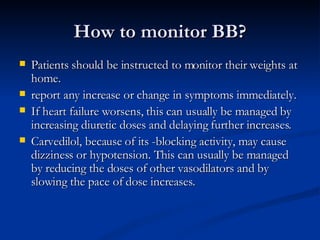
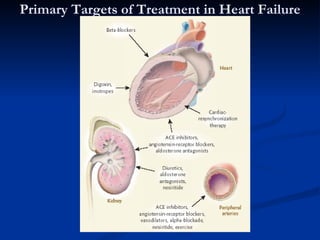
Congestive heart failure can be caused by conditions that weaken the heart muscle or overload it. The main symptoms are shortness of breath, fatigue, cough, and fluid retention. Treatment focuses on correcting reversible causes, reducing fluid overload with diuretics, and inhibiting the renin-angiotensin-aldosterone system with ACE inhibitors. Other medications like beta blockers, digitalis, and vasodilators may also be used depending on the individual case. Monitoring through physical exams, labs, and imaging can help guide management and prevent exacerbations.