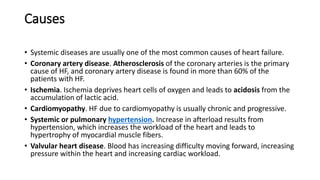
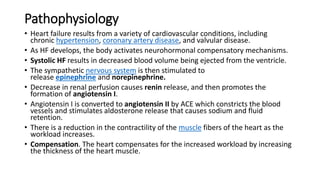
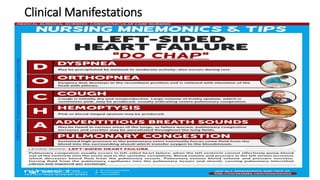
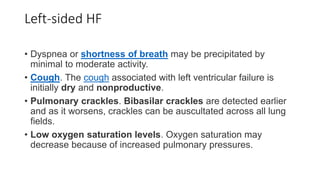
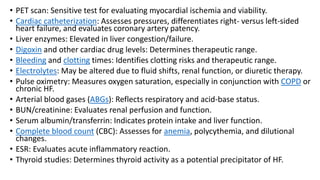
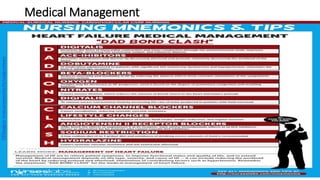
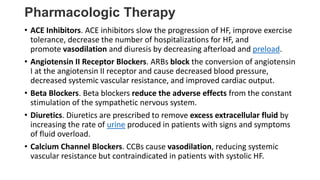
This document defines heart failure and describes its classification, causes, pathophysiology, clinical manifestations, diagnosis, management, and related nursing concerns. Heart failure occurs when the heart cannot pump enough blood to meet the body's needs and can be caused by conditions like coronary artery disease or cardiomyopathy. It is classified as left-sided or right-sided failure depending on the side of the heart affected. Management involves lifestyle changes, medications like ACE inhibitors and diuretics, and addressing complications. A key nursing concern is activity intolerance related to the heart's limited ability to meet oxygen demands during exercise.