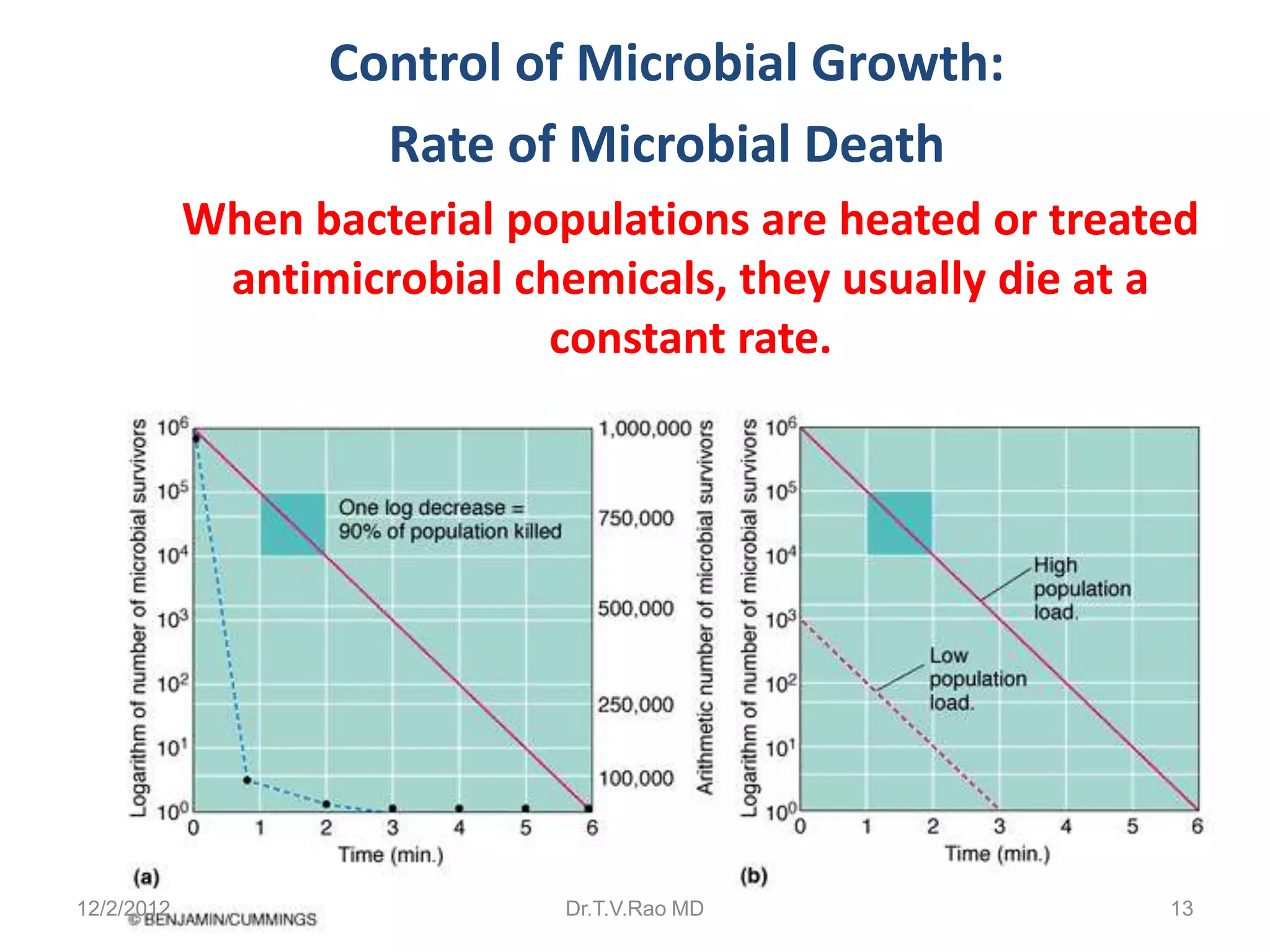
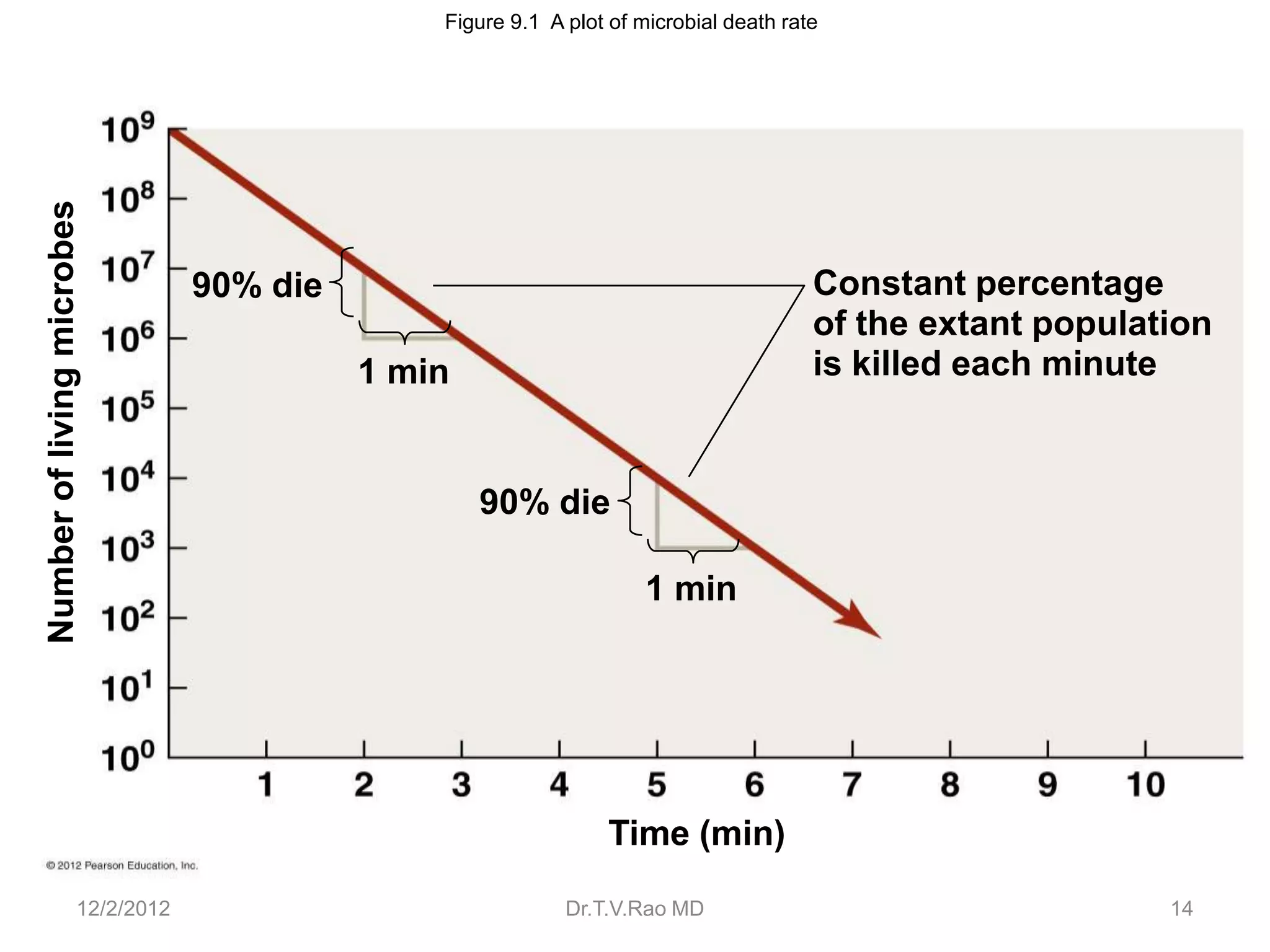
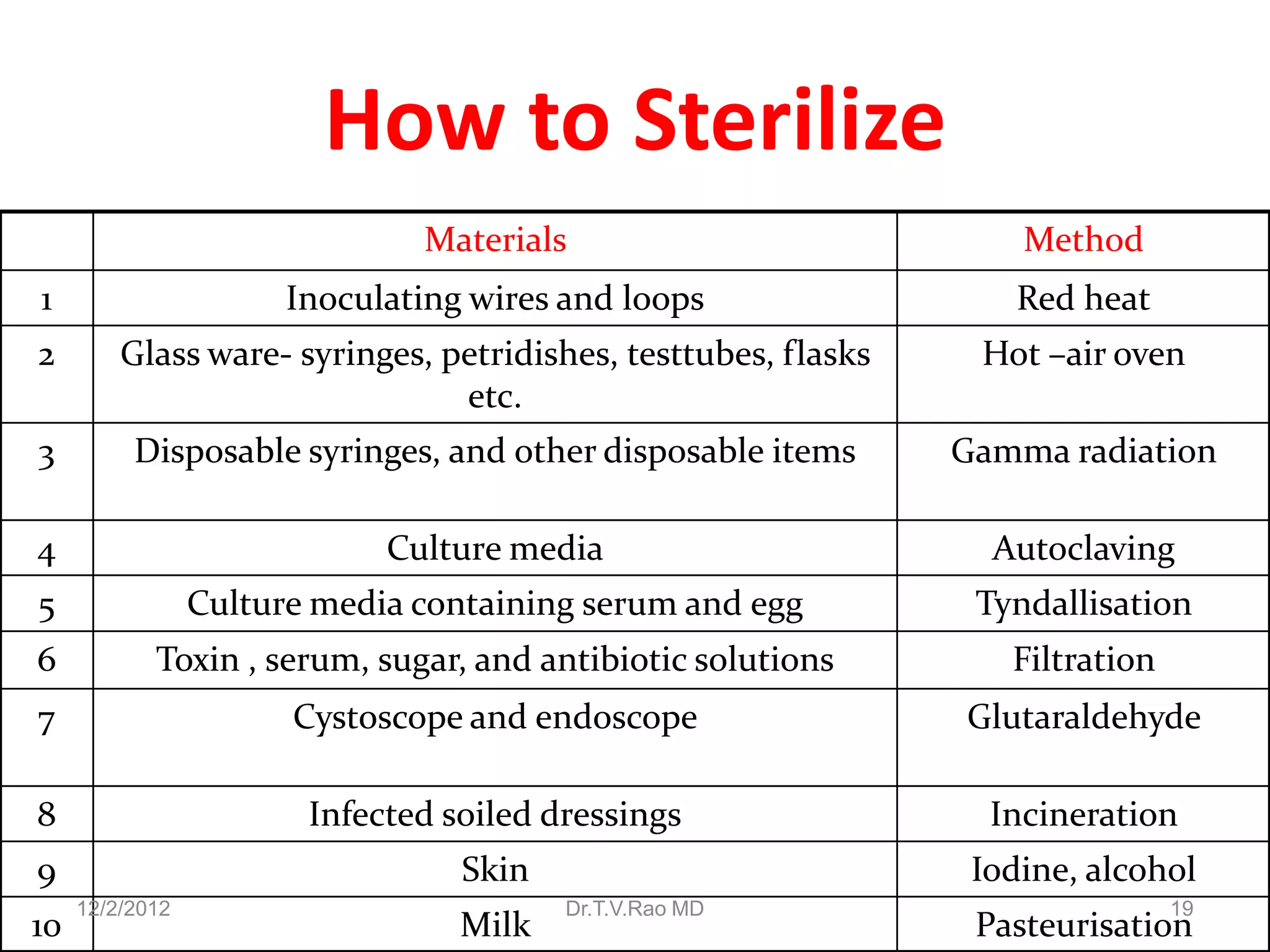
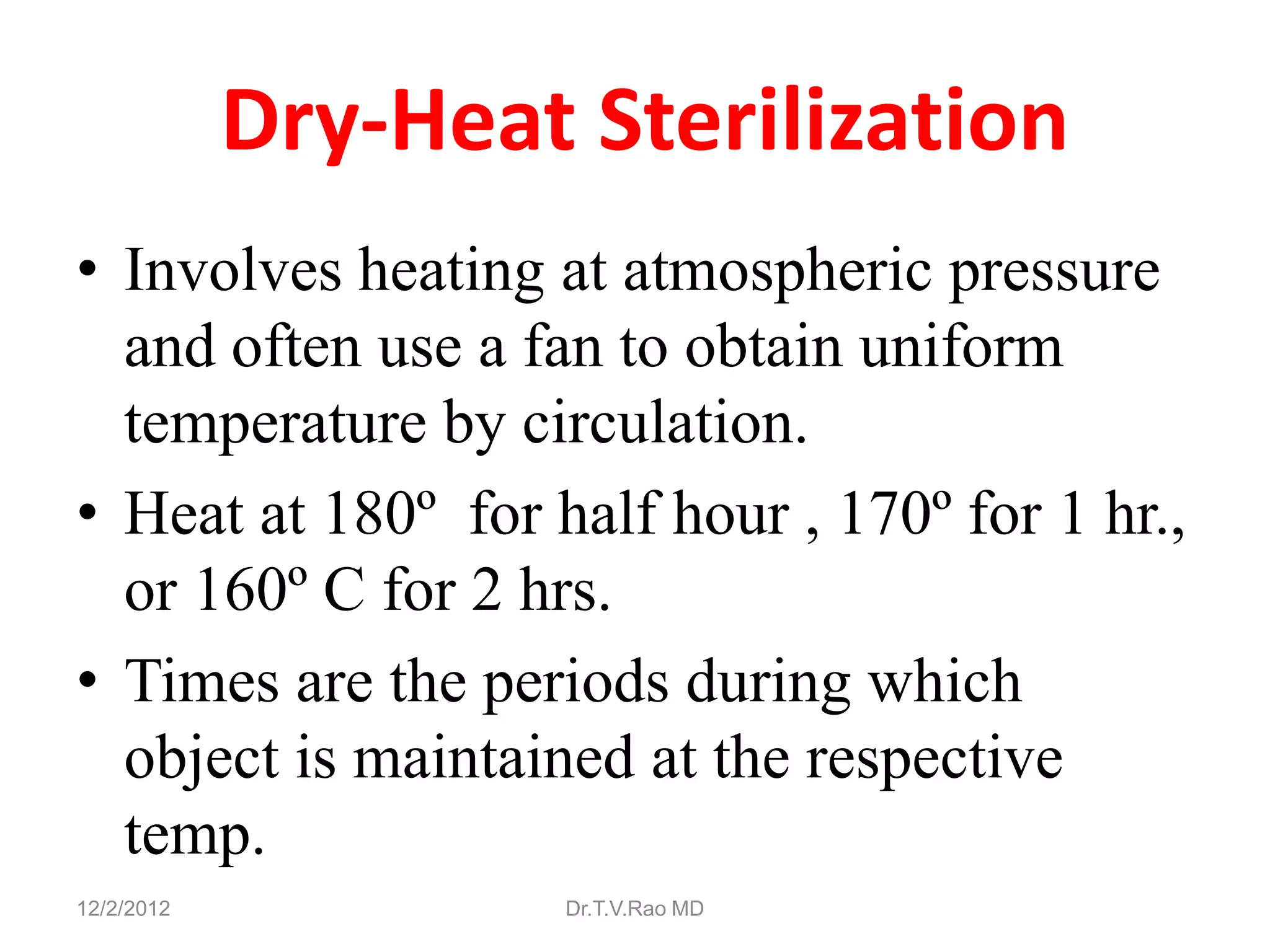
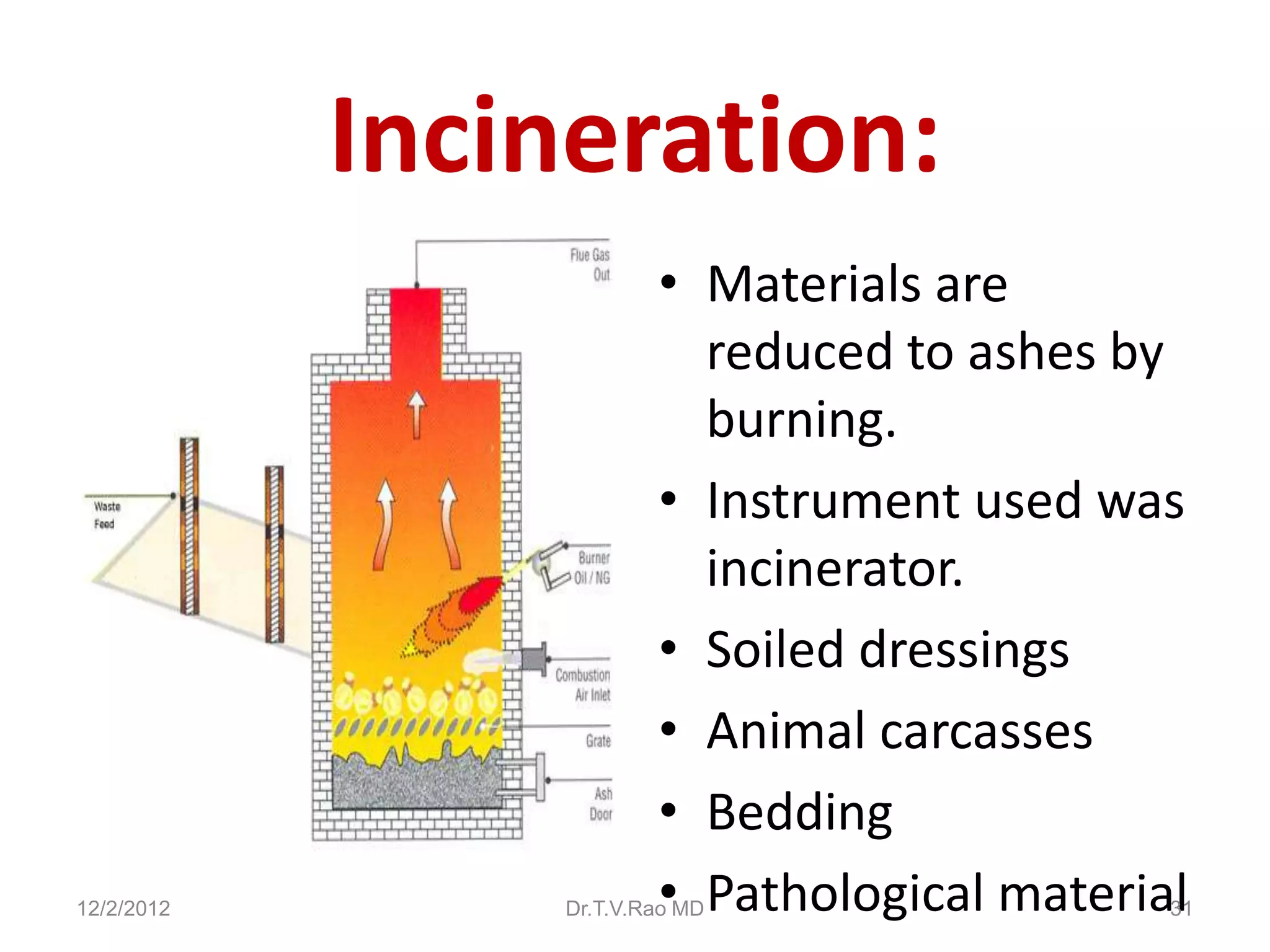
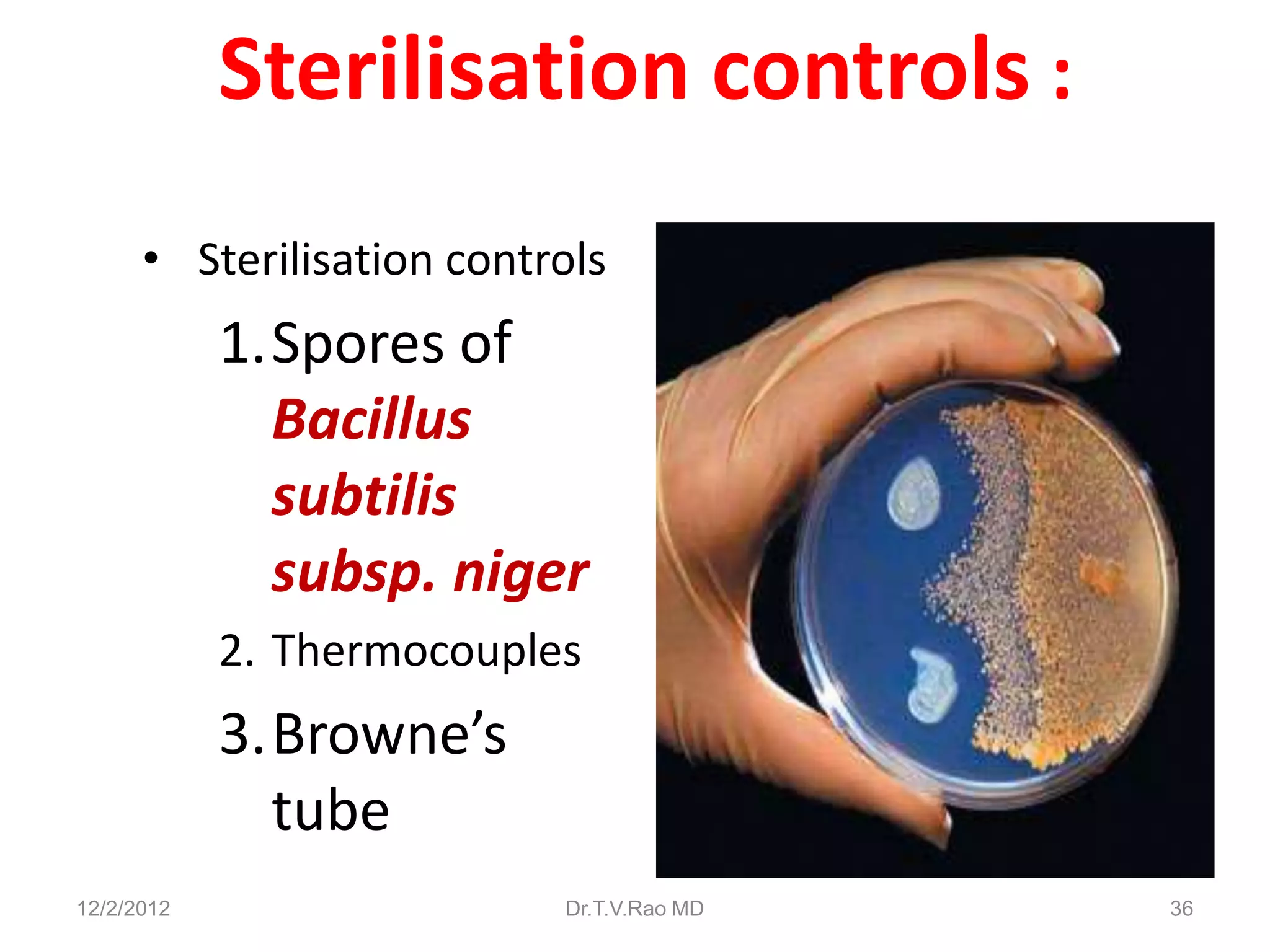
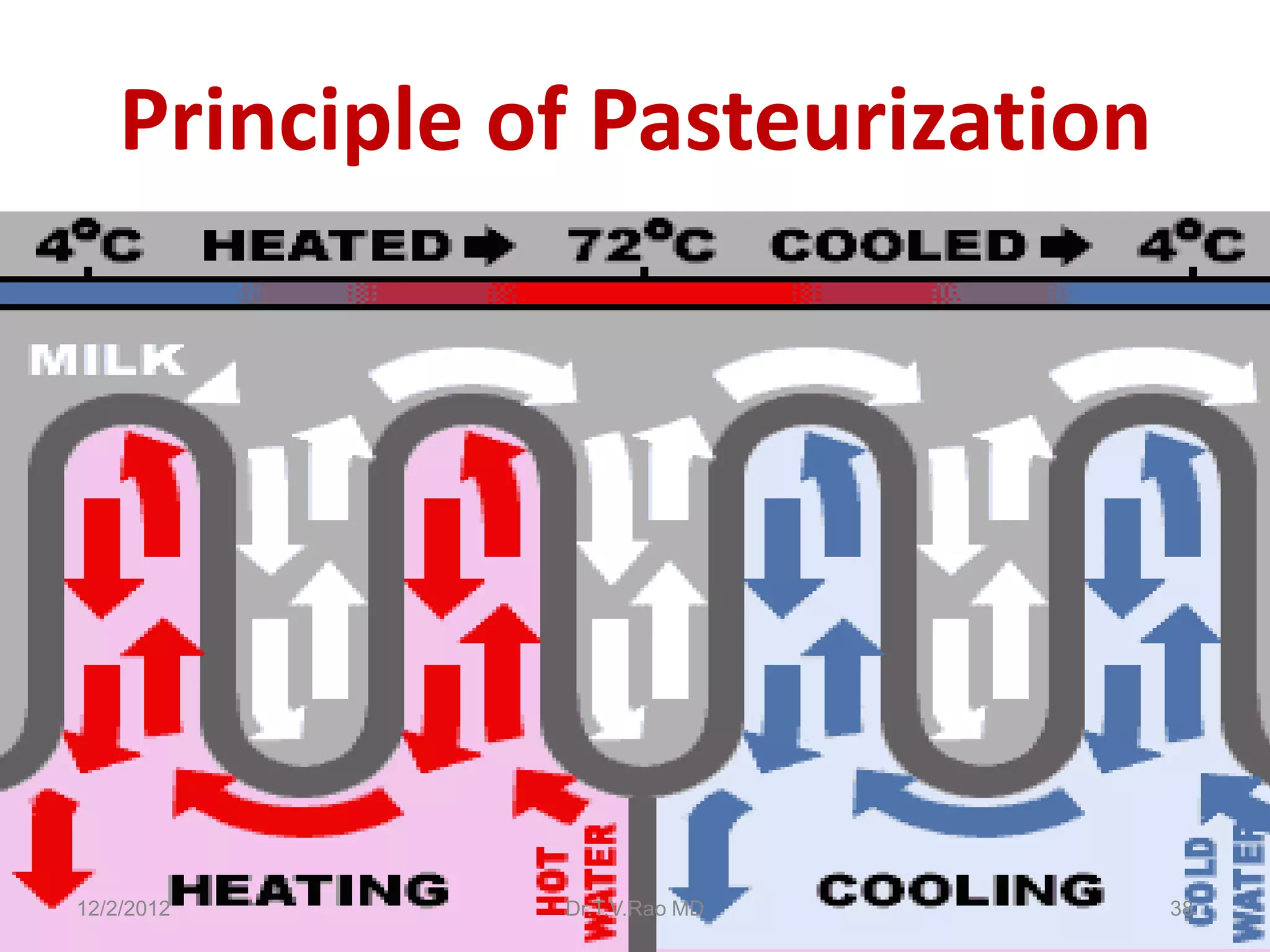
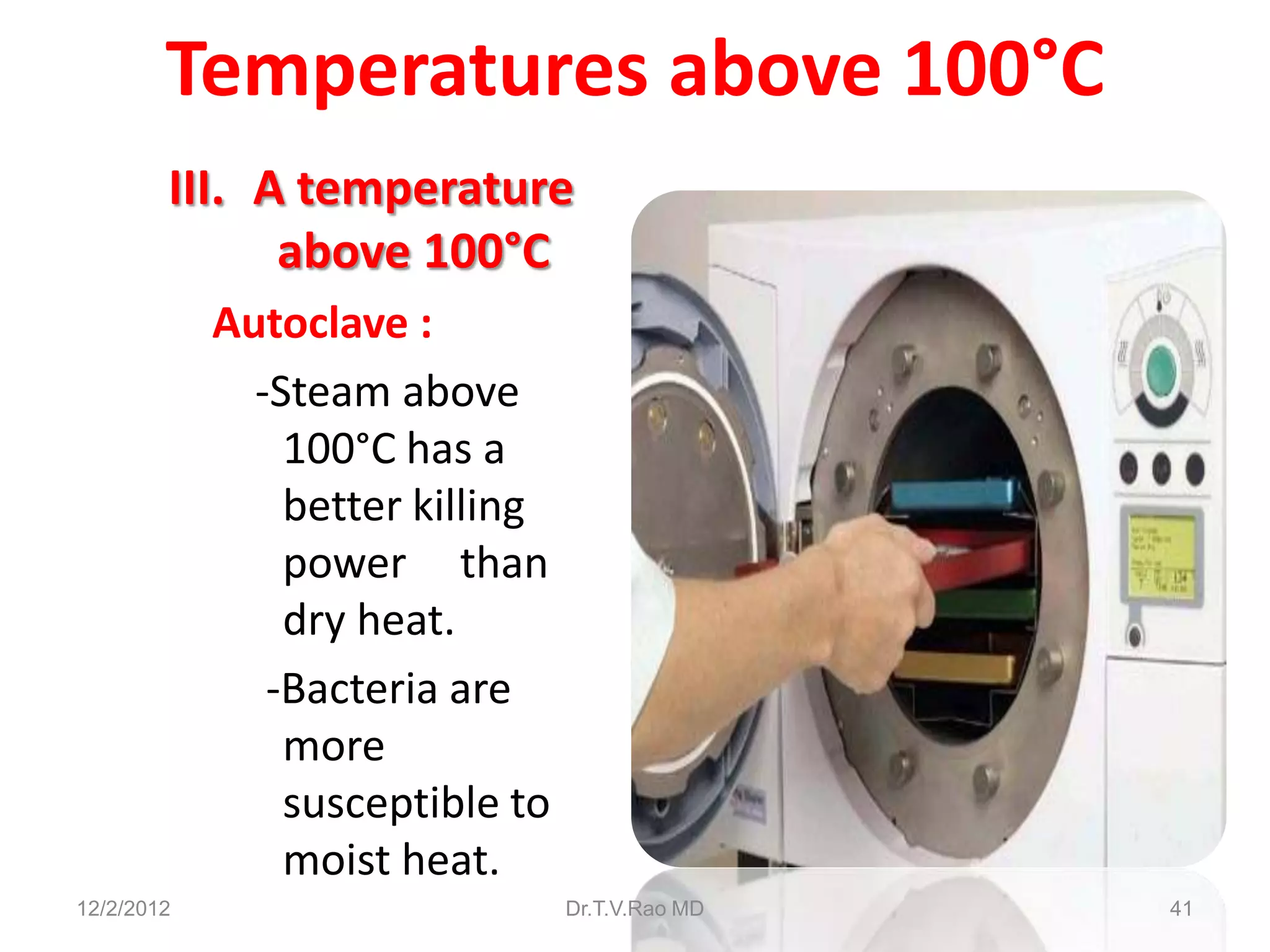
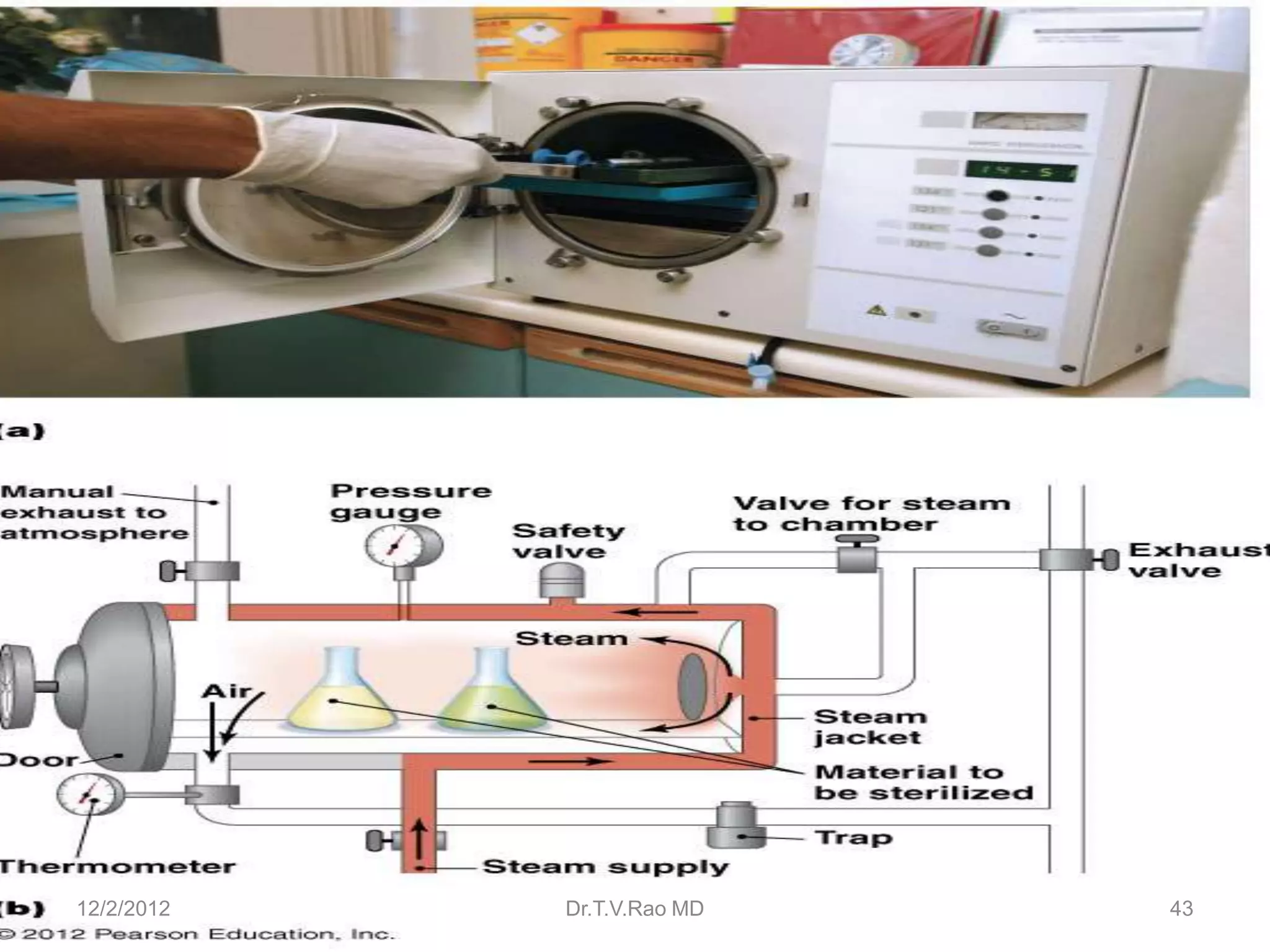
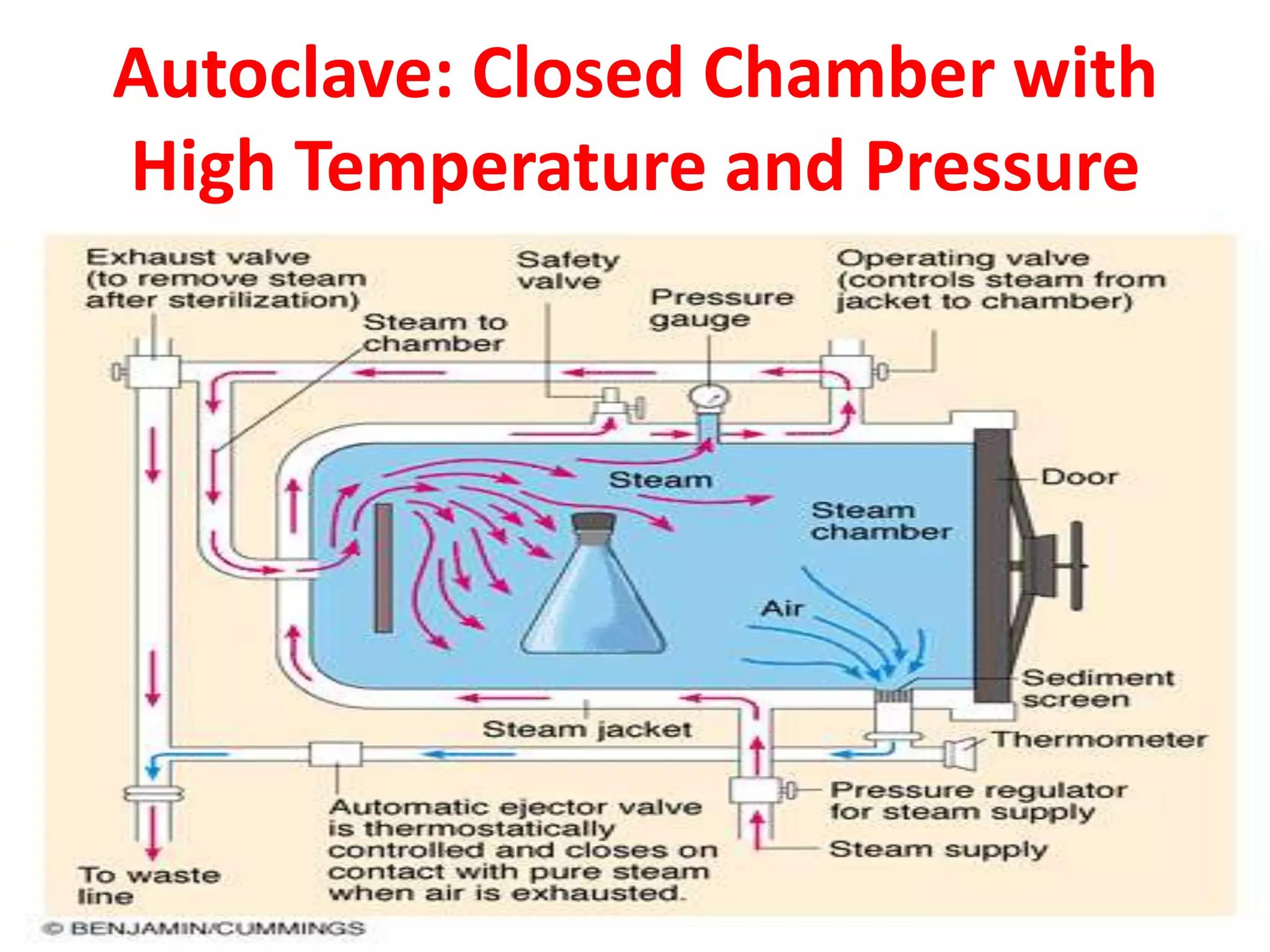
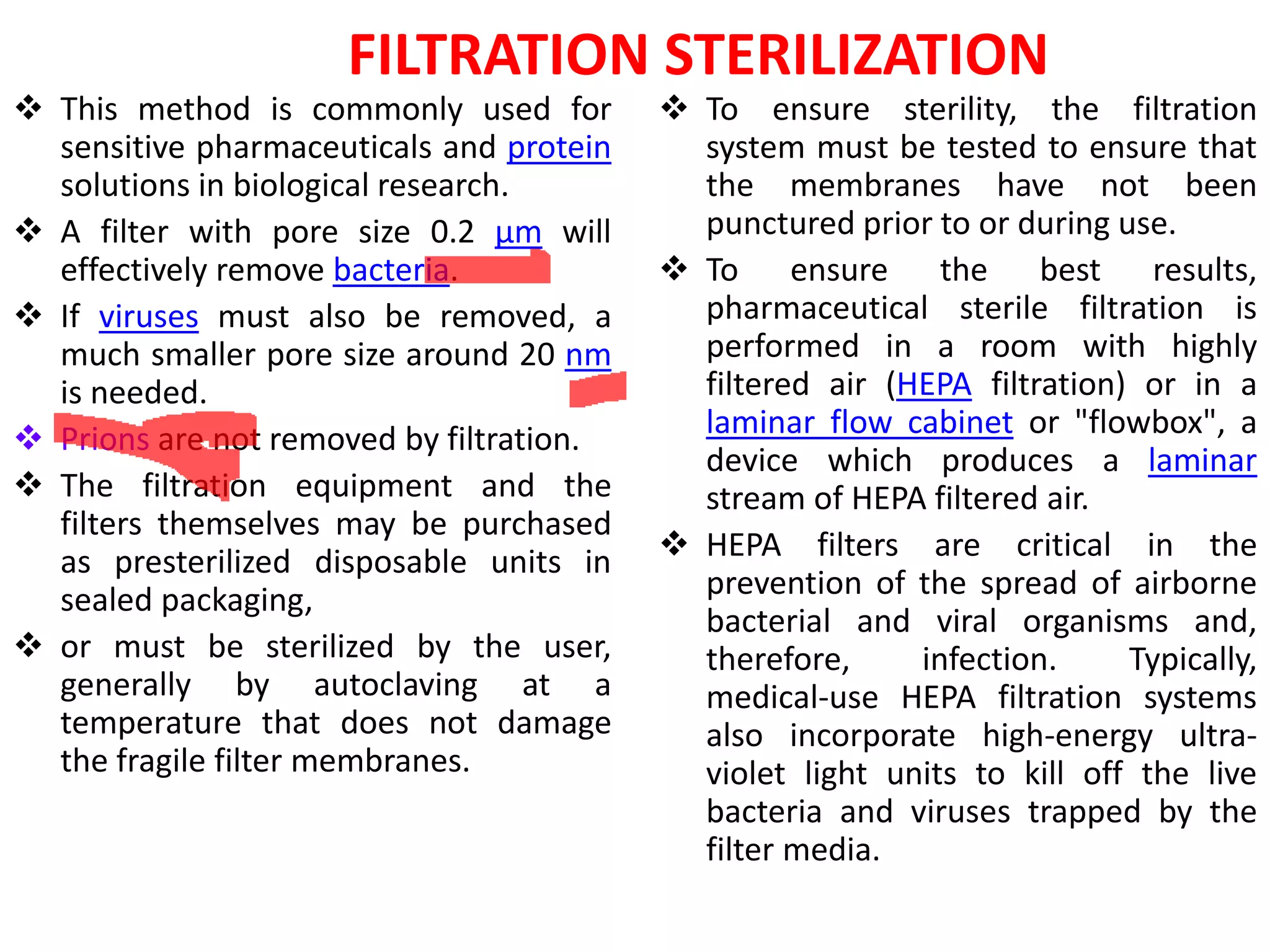
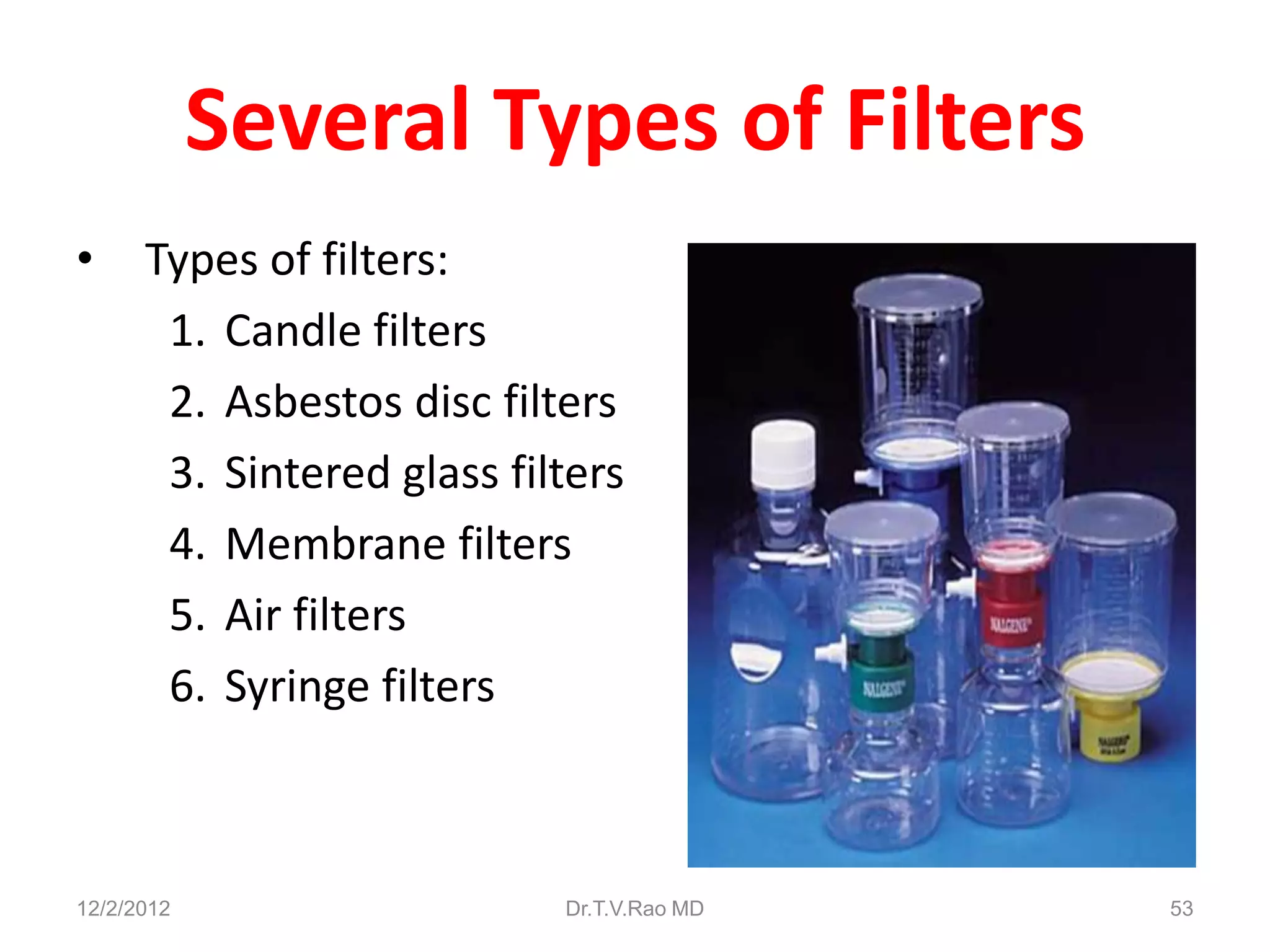
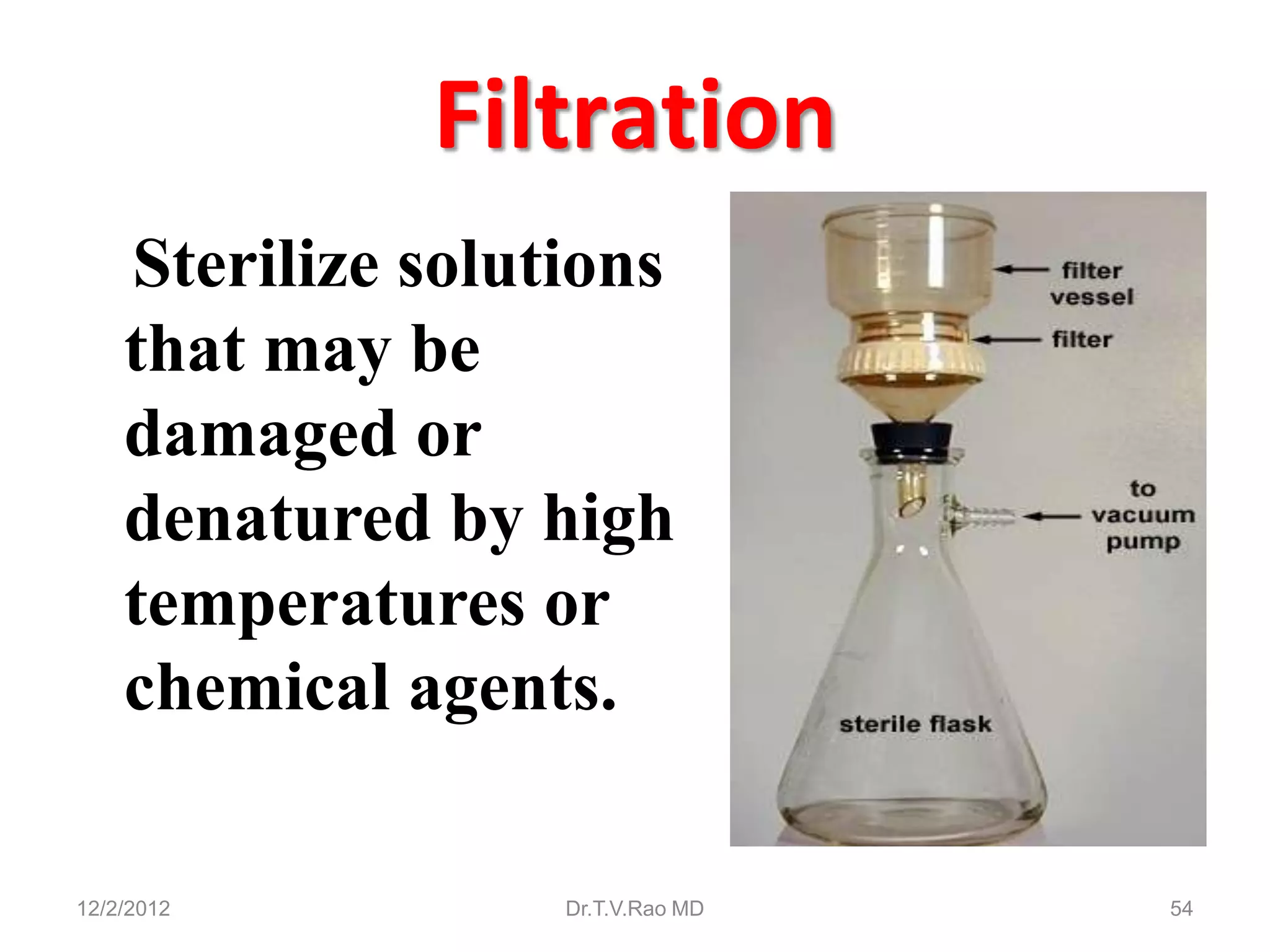
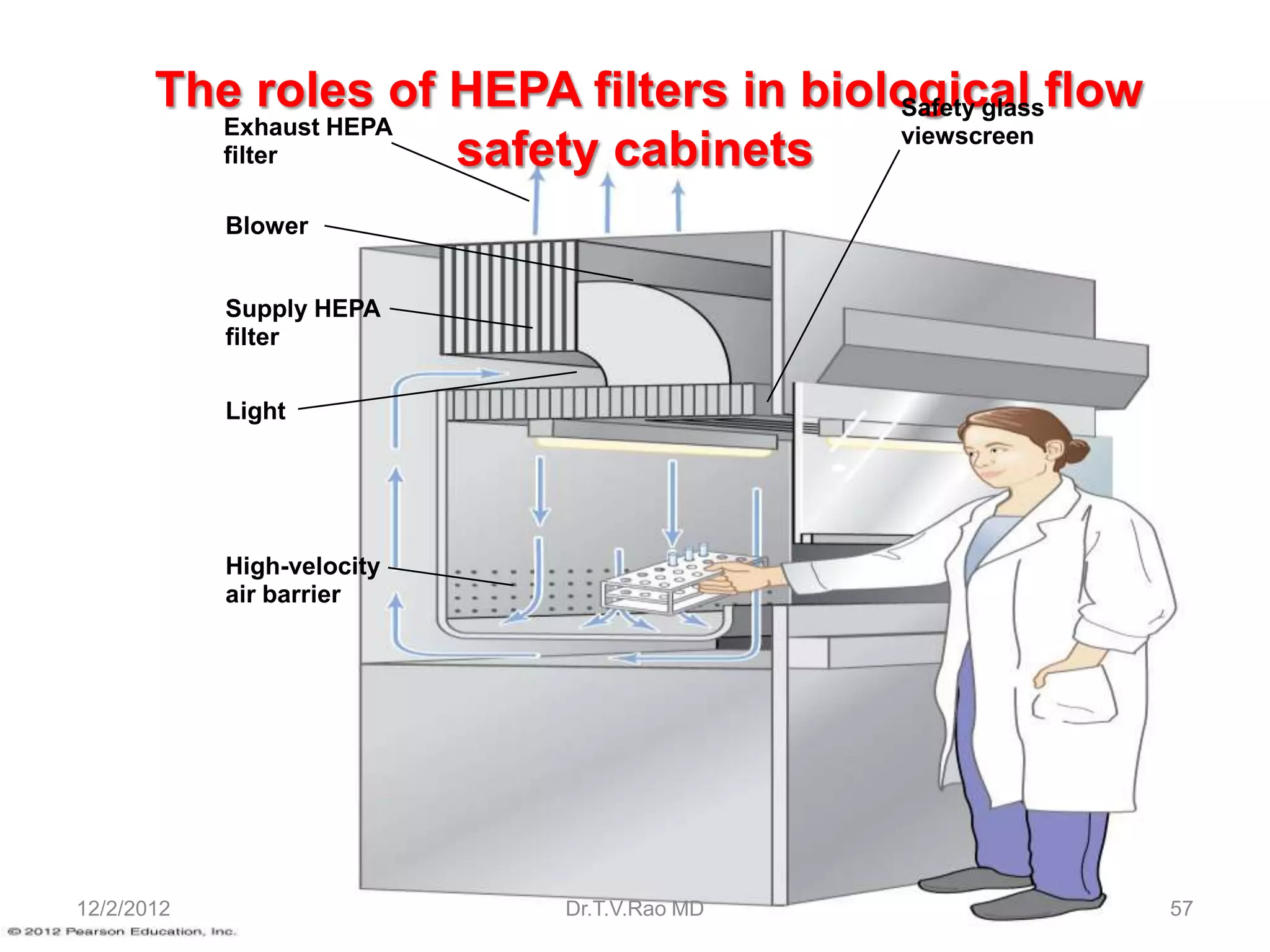
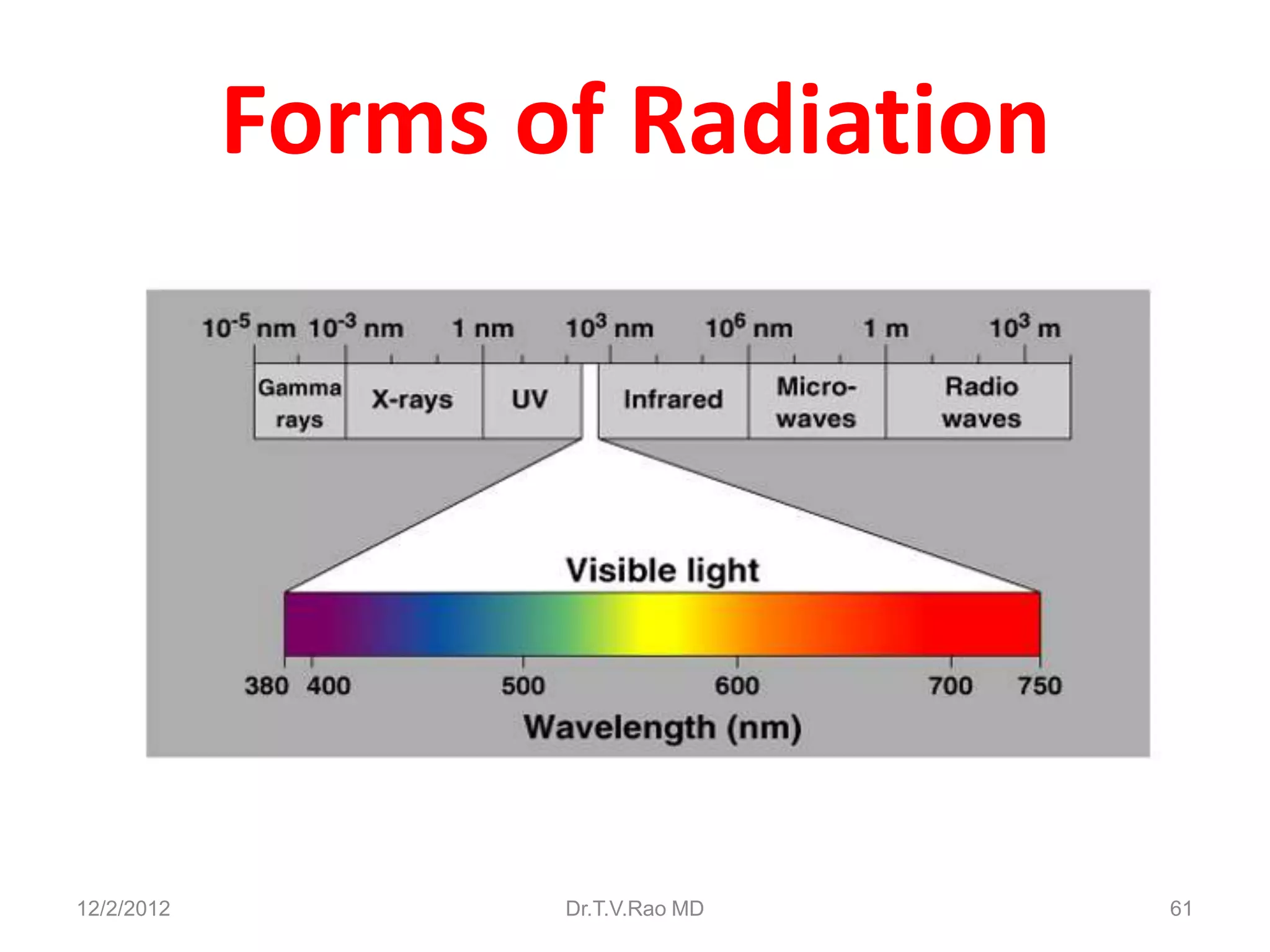
This document discusses various physical sterilization methods. It begins by explaining why sterilization is needed to remove or destroy microorganisms that can cause infection. It then describes different physical sterilization techniques like heat, radiation, and filtration. It provides details on specific heat-based methods for sterilizing different materials and lists the most common physical sterilization methods.