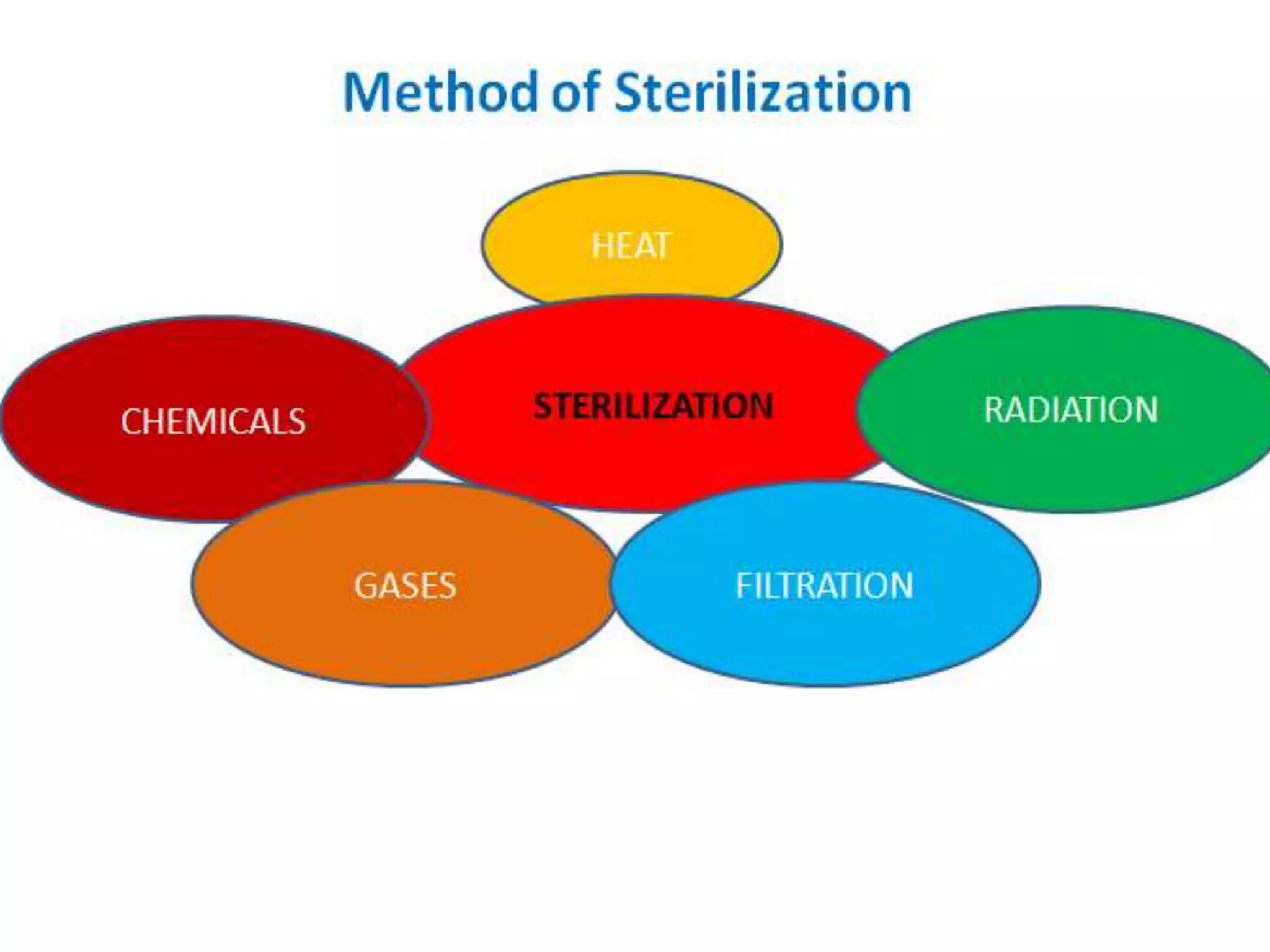
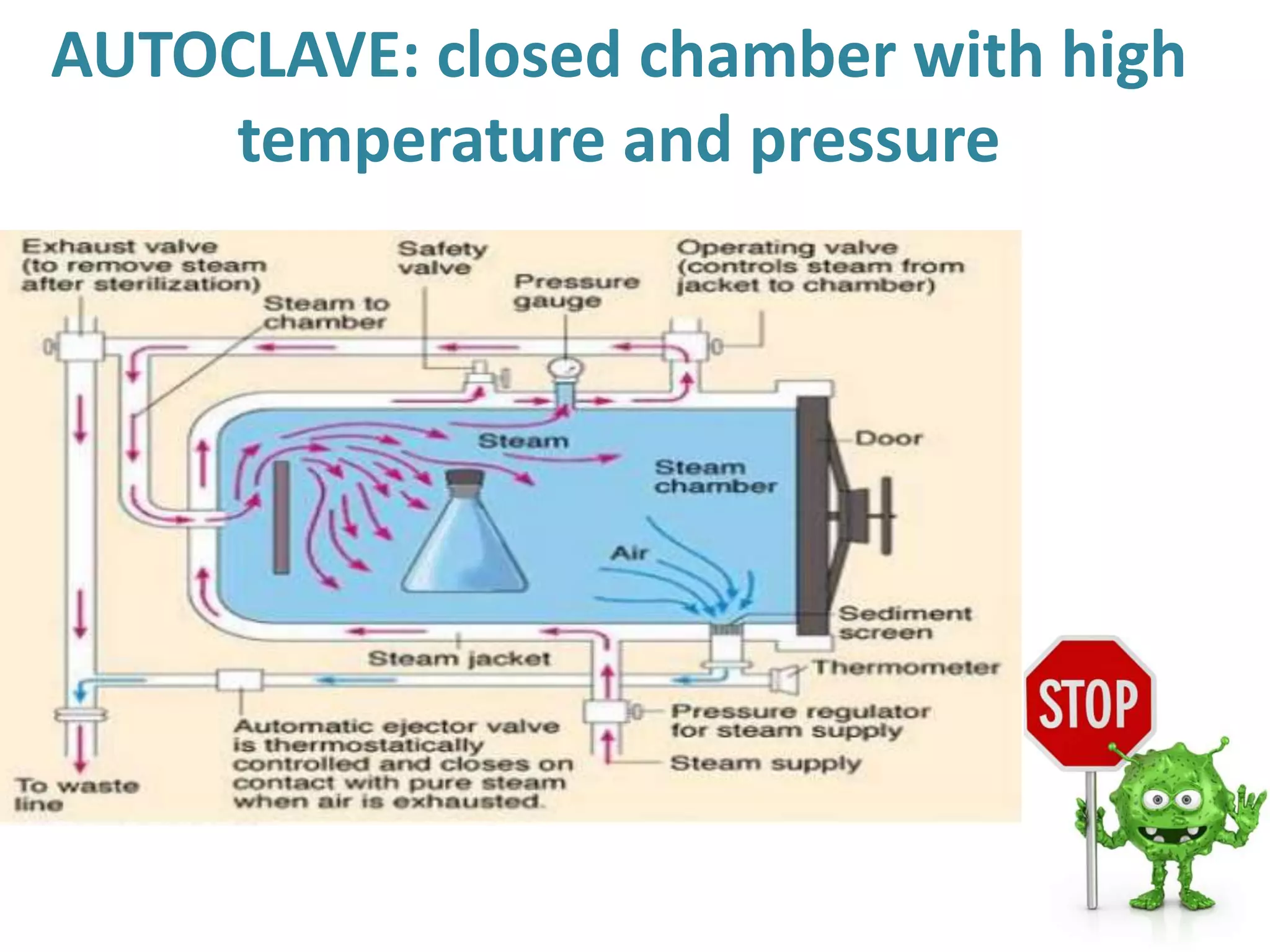
This document defines various sterilization, disinfection, and asepsis terms and describes different sterilization methods. It discusses sterilization using heat, including pasteurization which reduces microorganisms rather than eliminating them completely. Physical sterilization methods like hot air ovens and chemical methods are also outlined. The document provides details on factors influencing the efficacy of sterilization and classifications of different sterilization techniques.