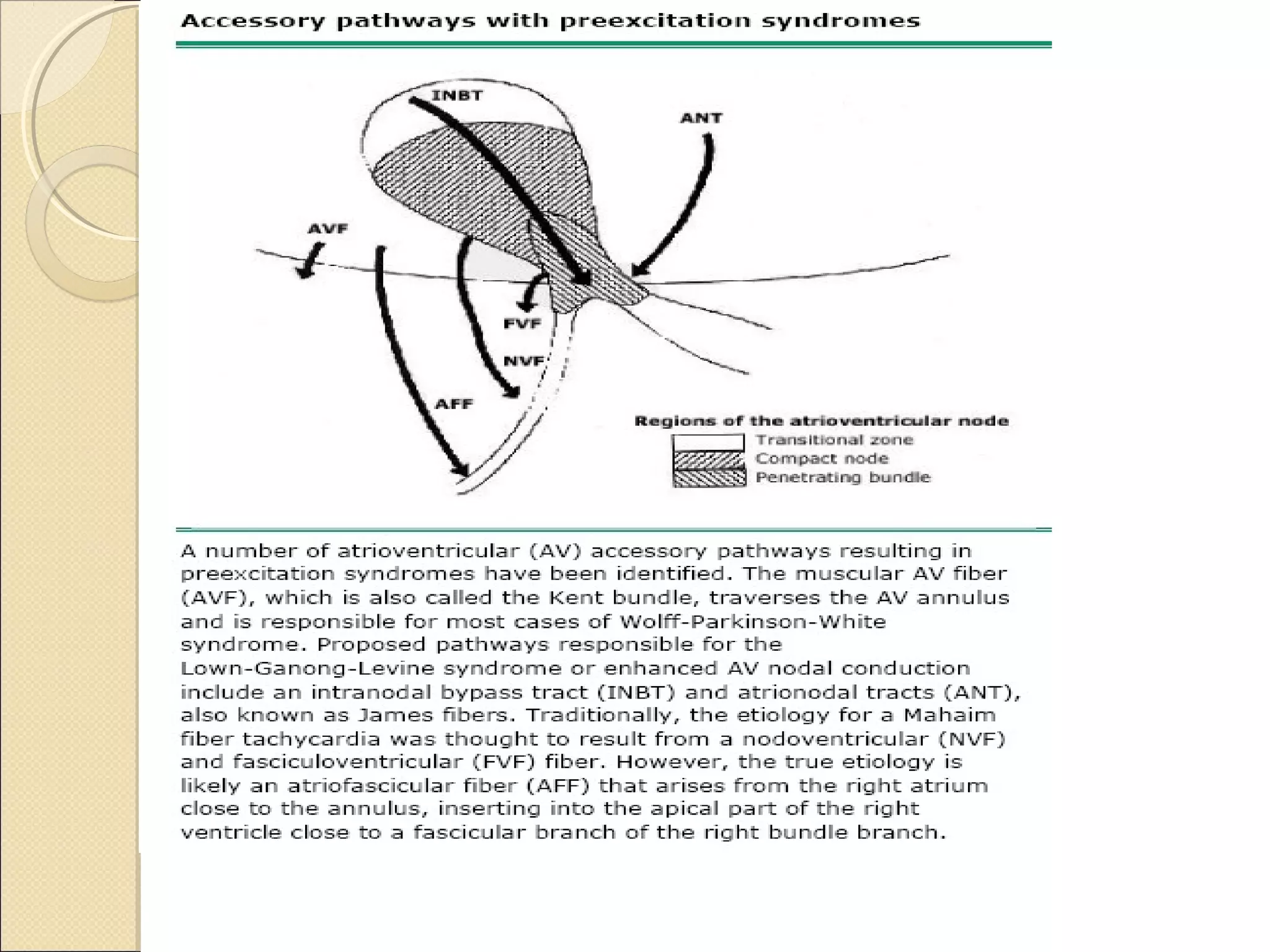
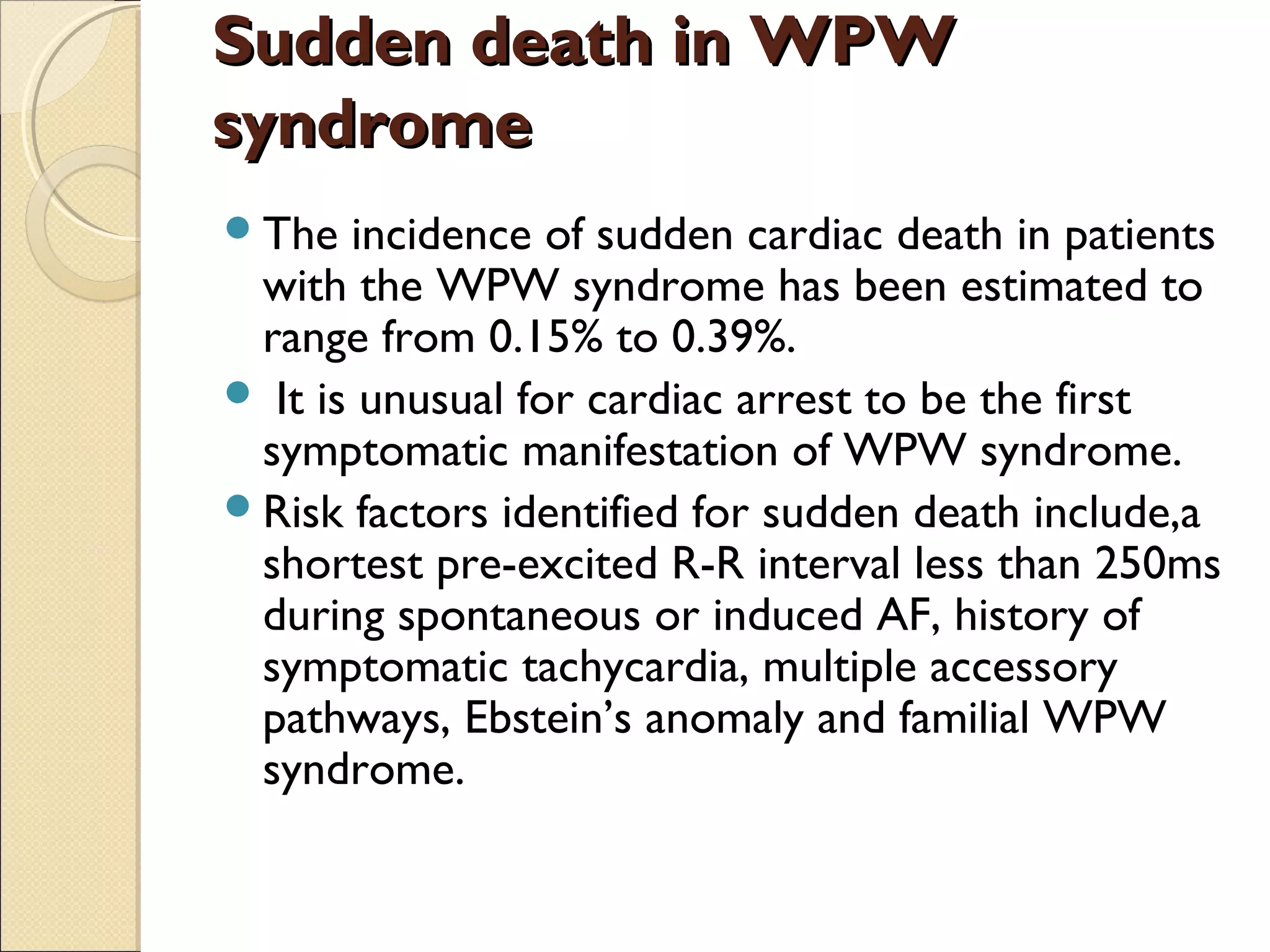
The document provides a comprehensive overview of Wolff-Parkinson-White (WPW) syndrome, covering its historical background, clinical presentation, pathophysiology, symptoms, and electrophysiological assessment. WPW is characterized by an accessory pathway that allows for abnormal electrical conduction, resulting in pre-excitation of the ventricles and potential tachycardia. Key advancements in diagnosis and treatment, including catheter ablation, are also highlighted, along with risk factors for sudden death associated with the syndrome.
































![Polarity of QRS QRS
AXIS
DELT
A
AXIS
V1 V2 V3
Antero septal
- - - NORMAL NORMAL
Rt lat
- - - LEFT
[ -60]
LEFT
[ -60]
Rt postseptal
- + + LEFT [ -30] LEFT[ -60]
Lt postseptal
+ + + LEFT[ -30] LEFT[ -60]](https://image.slidesharecdn.com/wpwsyndrome-130718092259-phpapp02/75/Wpw-syndrome-46-2048.jpg)
![DELTA IN
V1
QRS IN V1 QRS IN V2
RT POST
SEPTAL
ISO or NEGATIVE DOMINANTLY
NEGATIVE
POSITIVE
LT POST
SEPTAL
POSITVE
[ALWAYS]
DOMINANTLY
POSITIVE or
equiphasic
positive](https://image.slidesharecdn.com/wpwsyndrome-130718092259-phpapp02/75/Wpw-syndrome-47-2048.jpg)
























