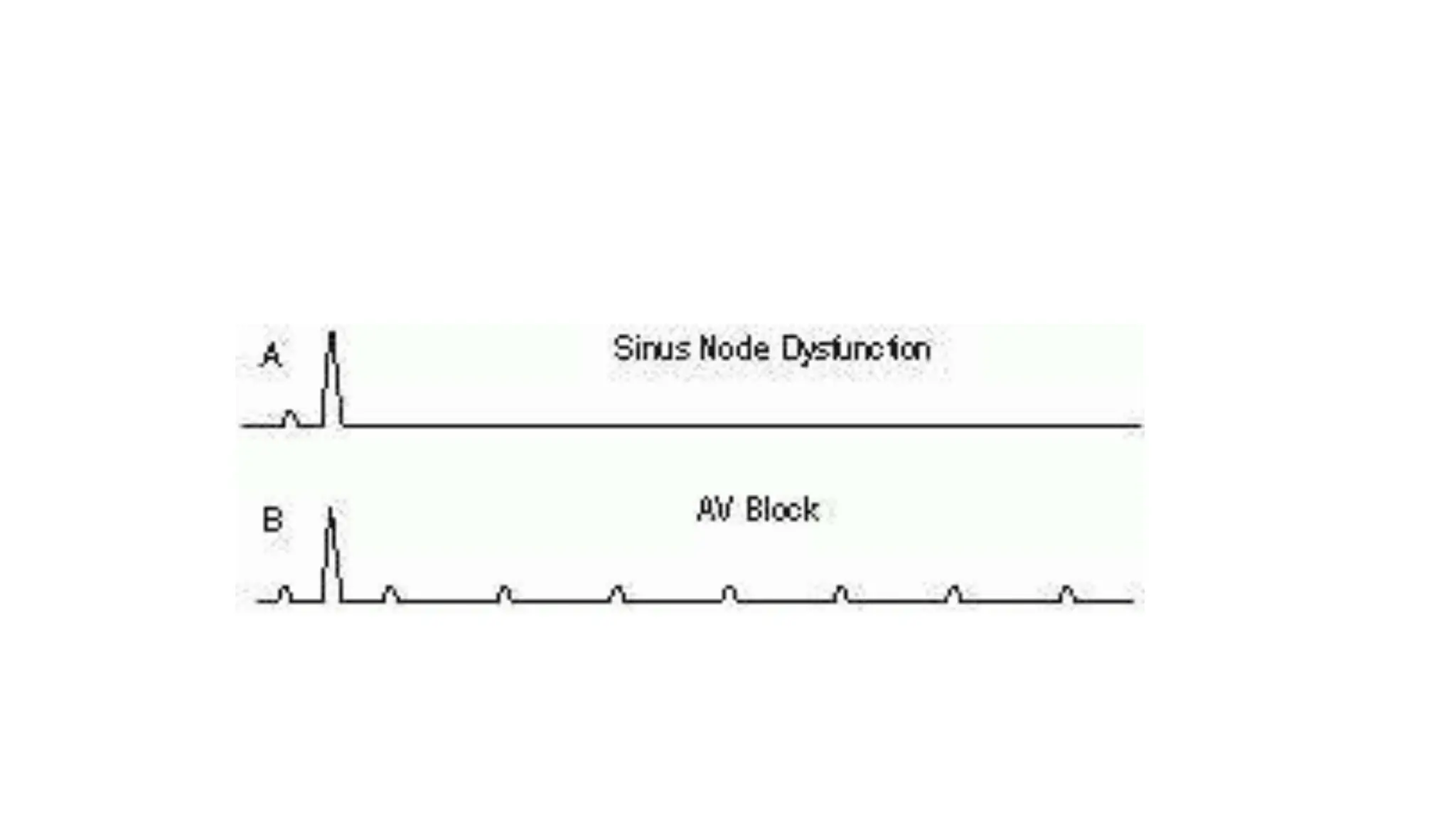
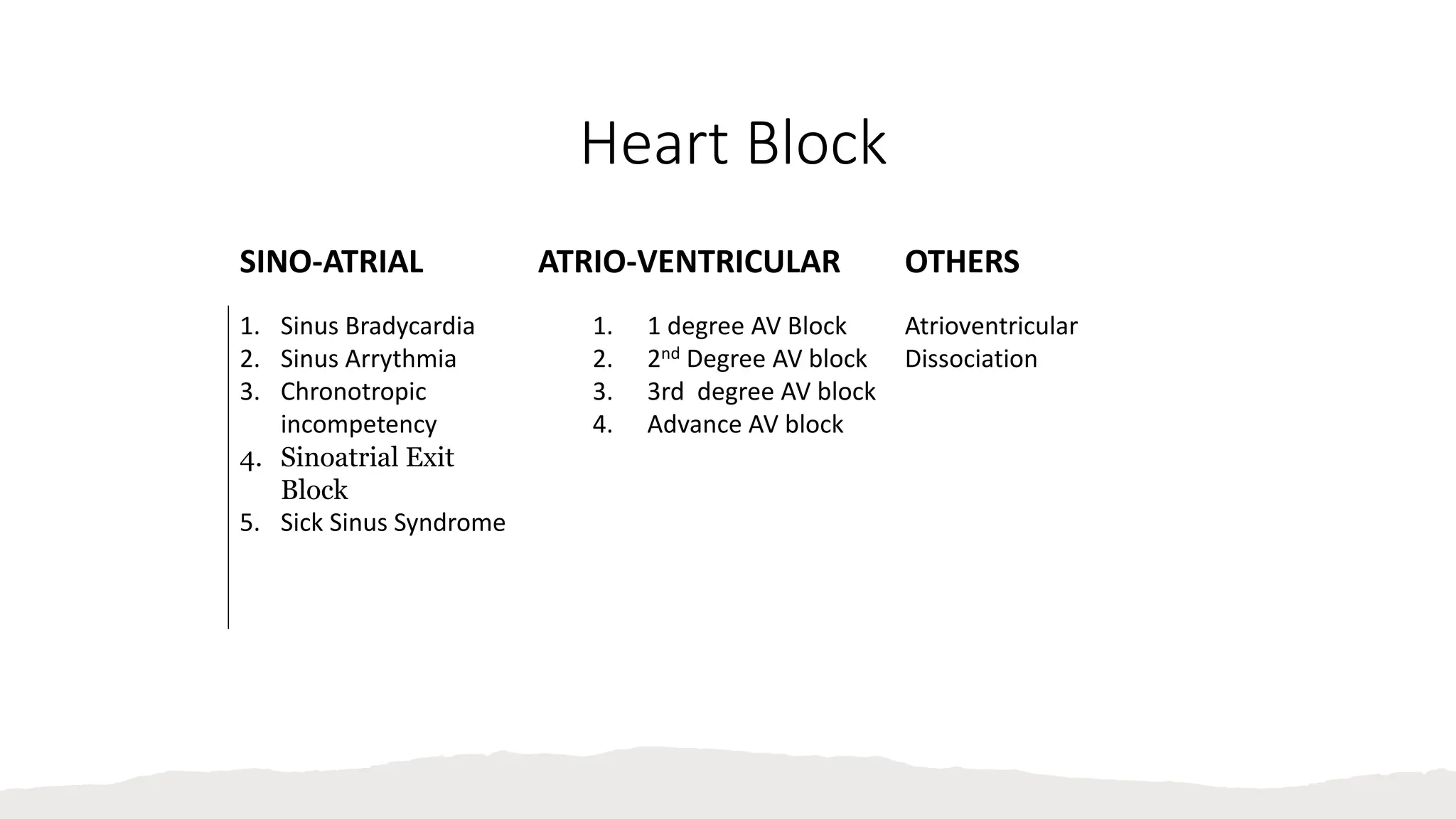
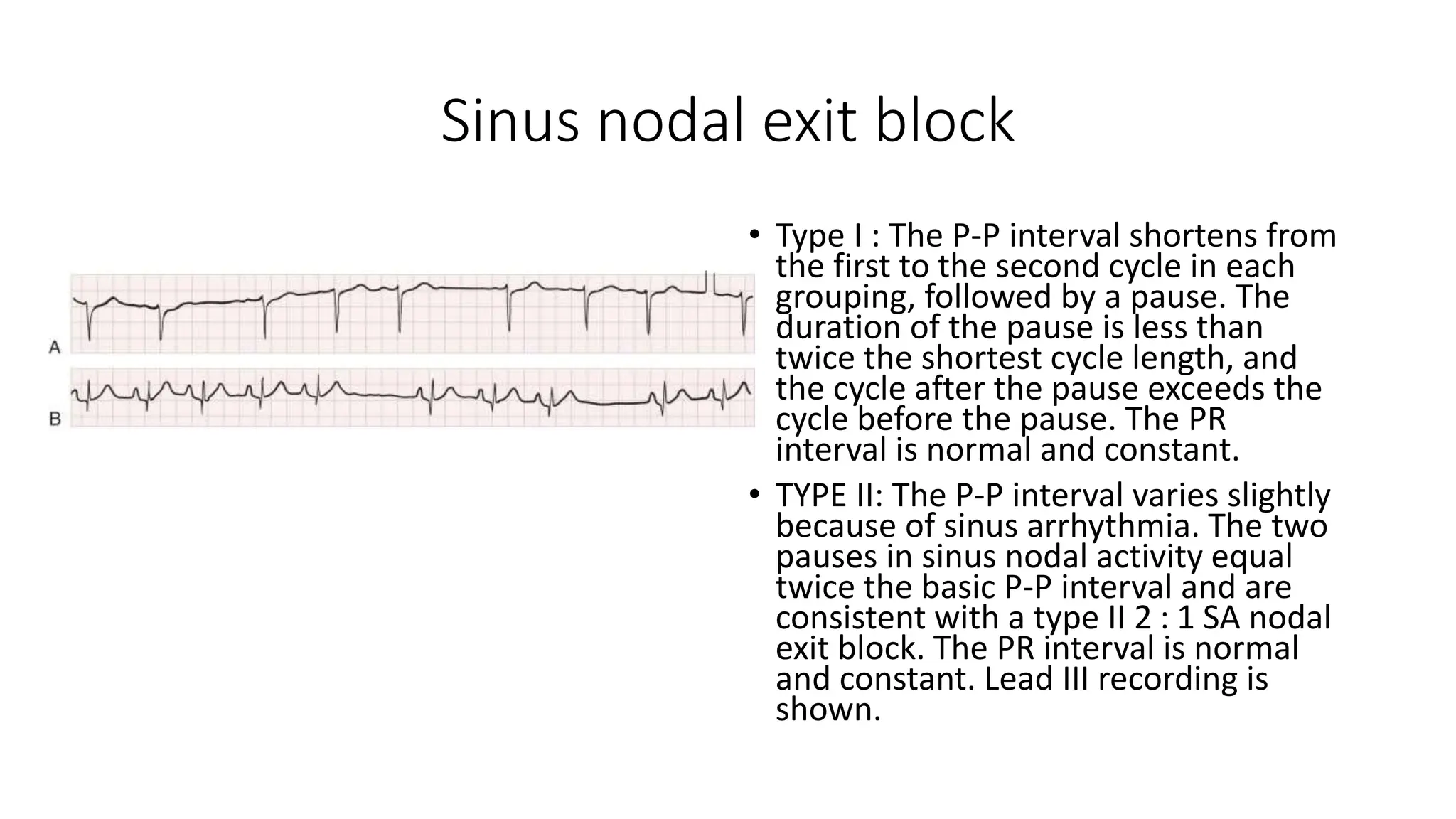
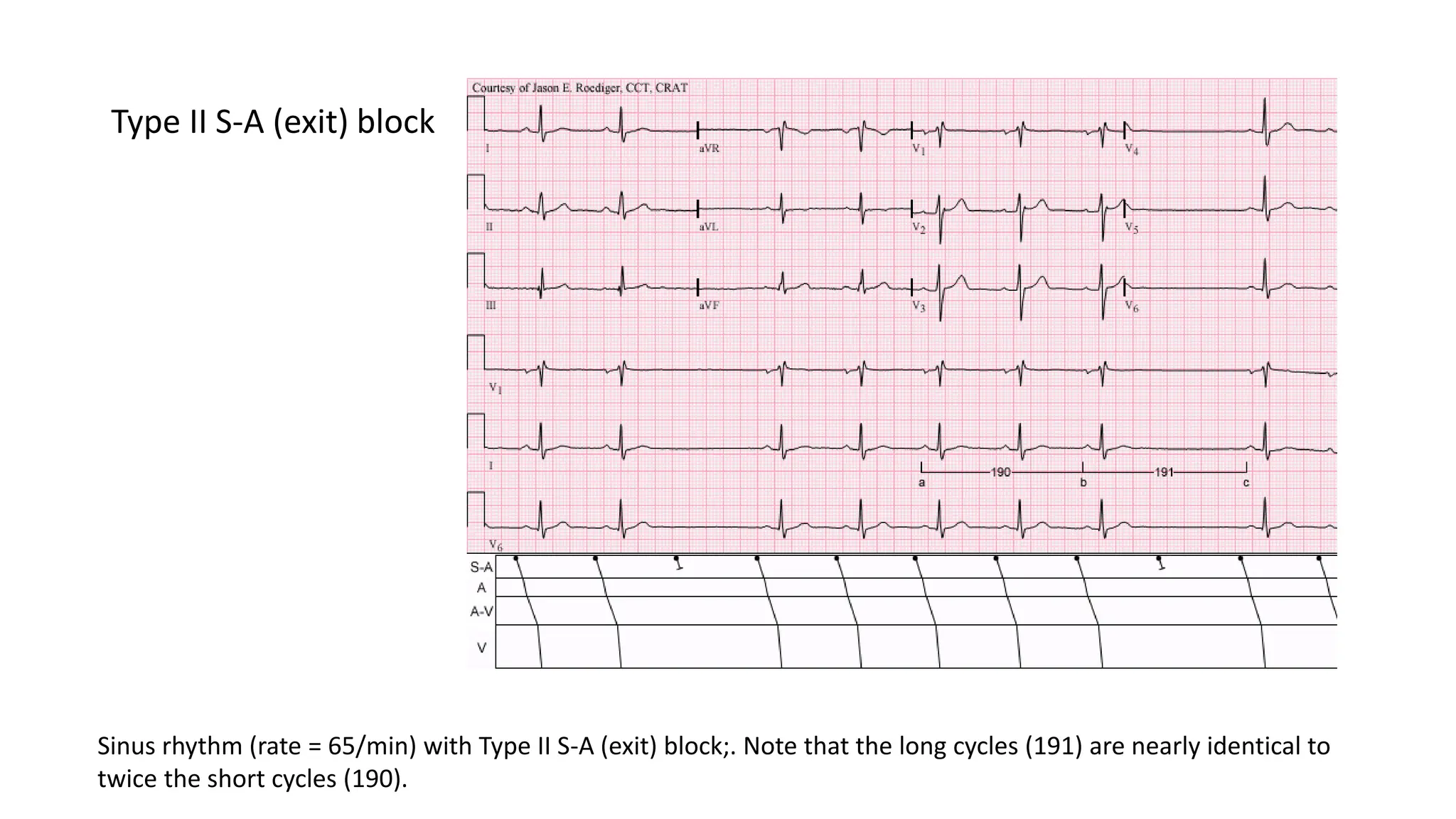
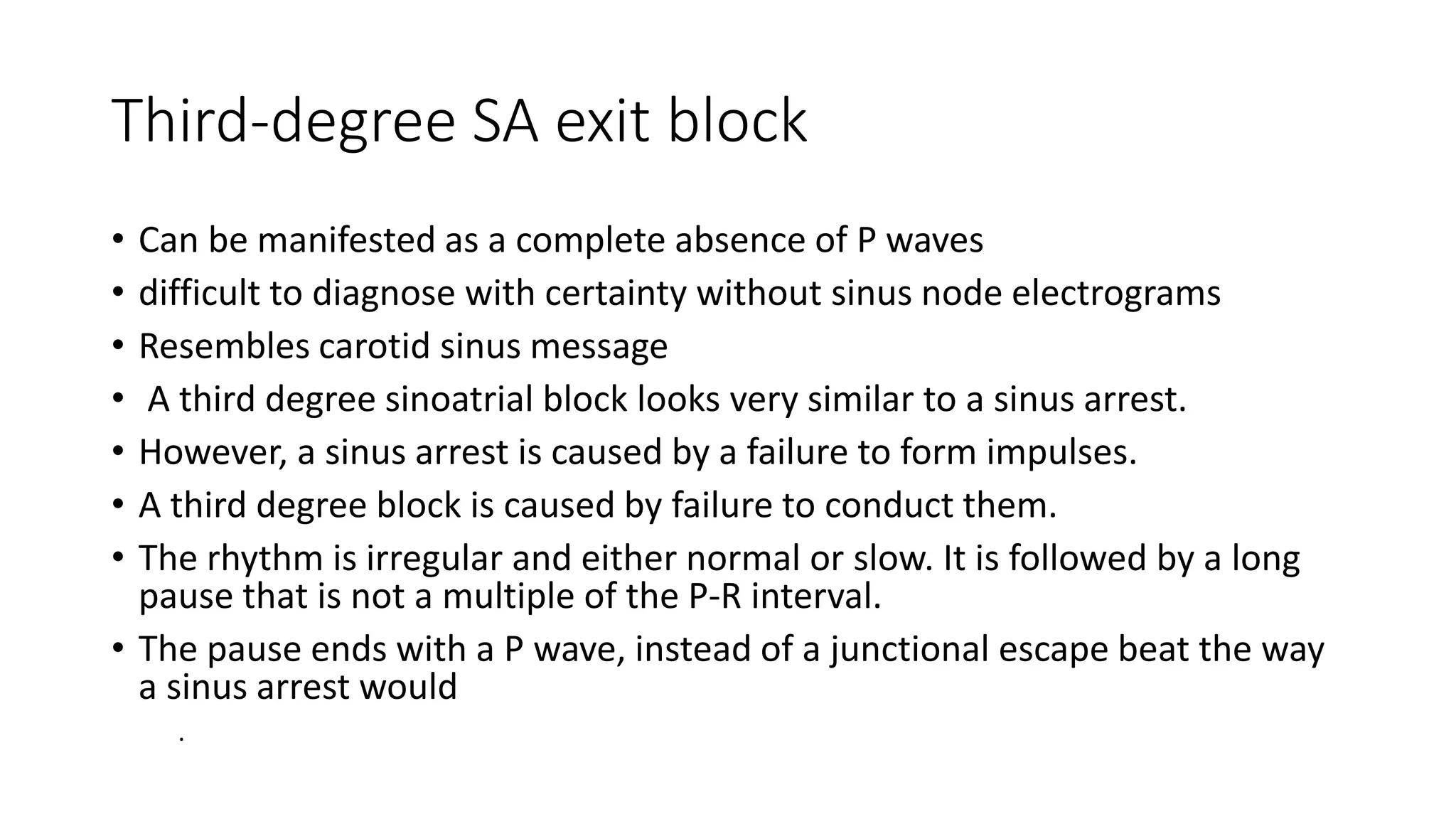
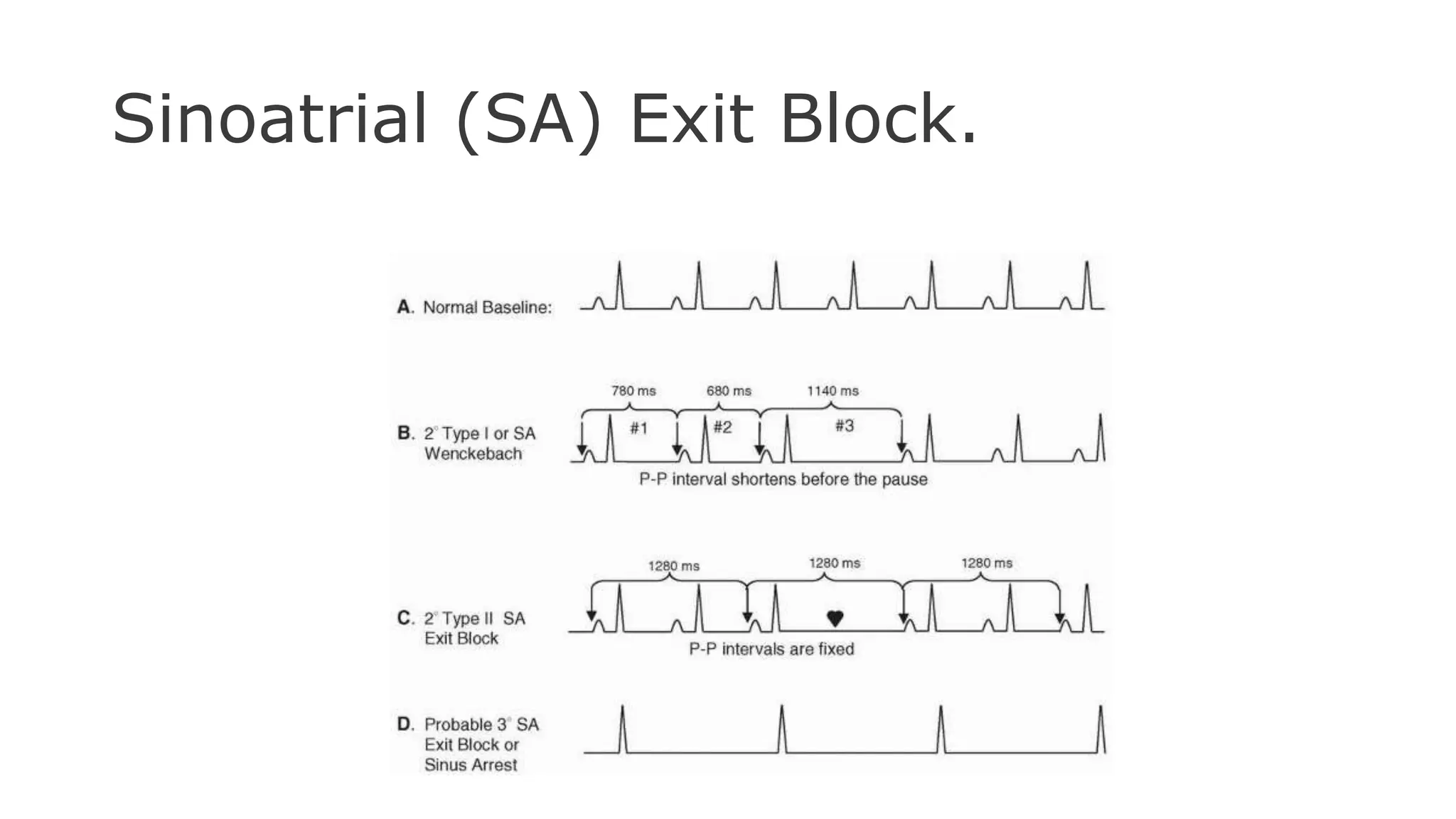
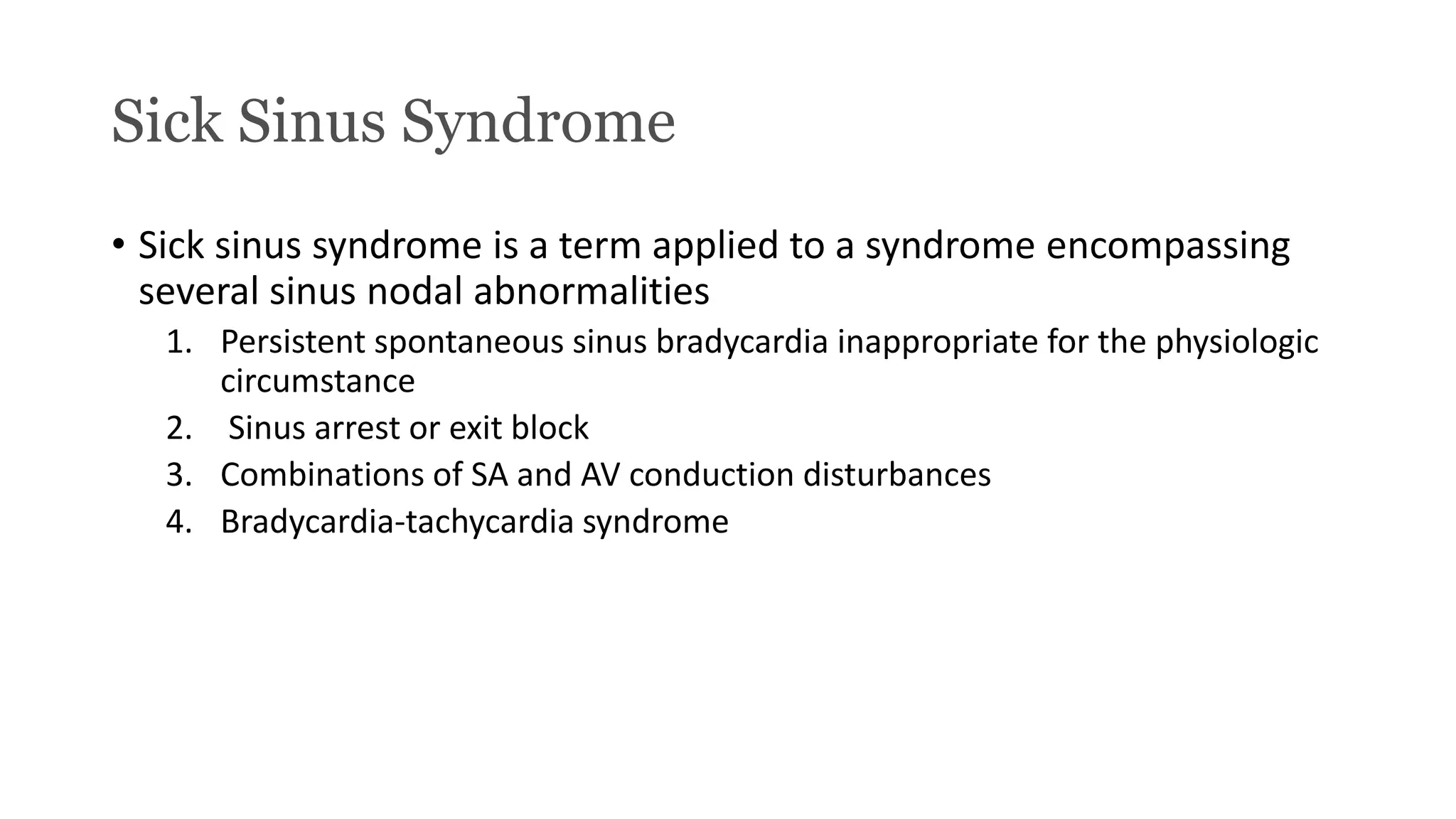
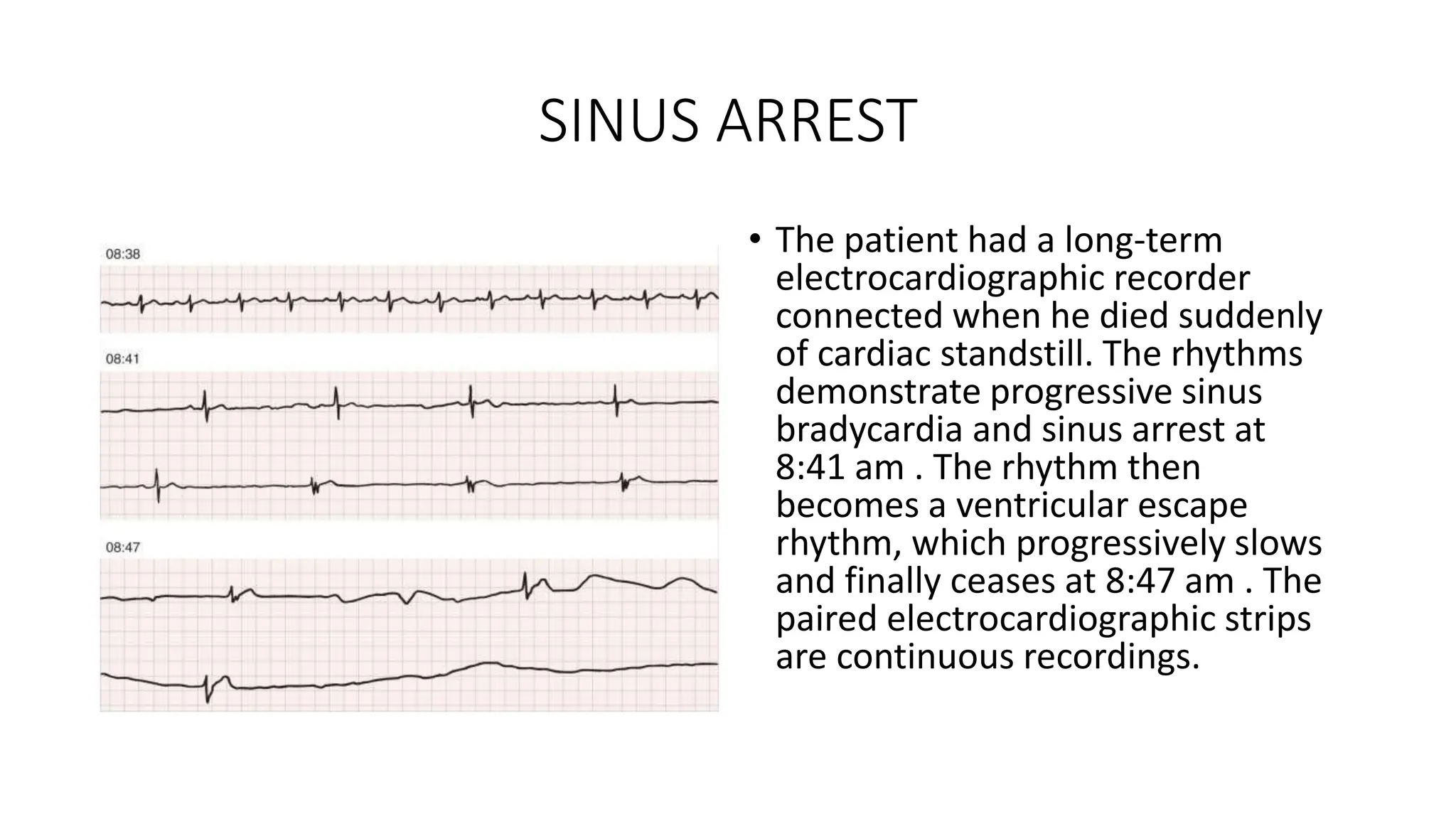
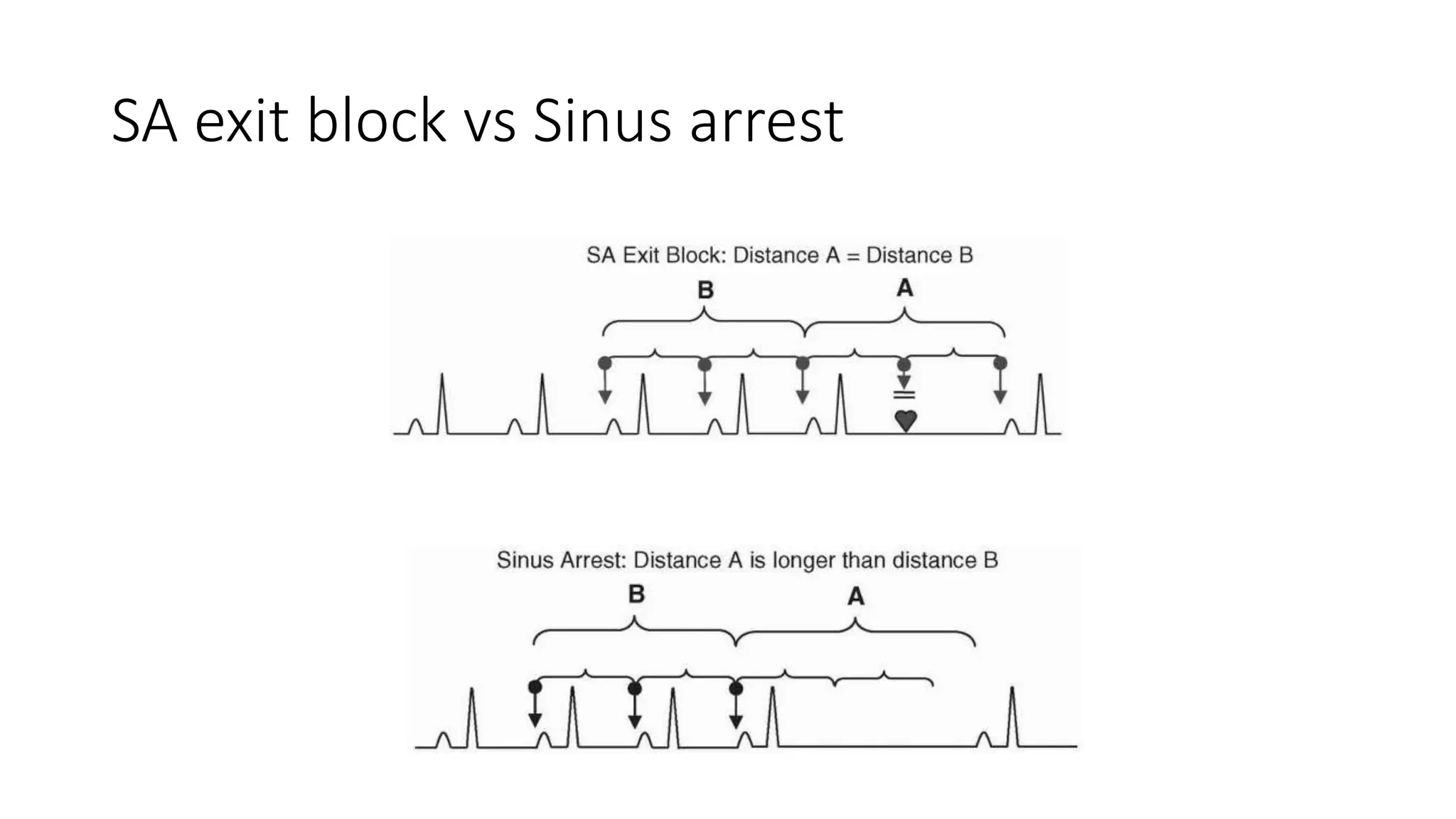
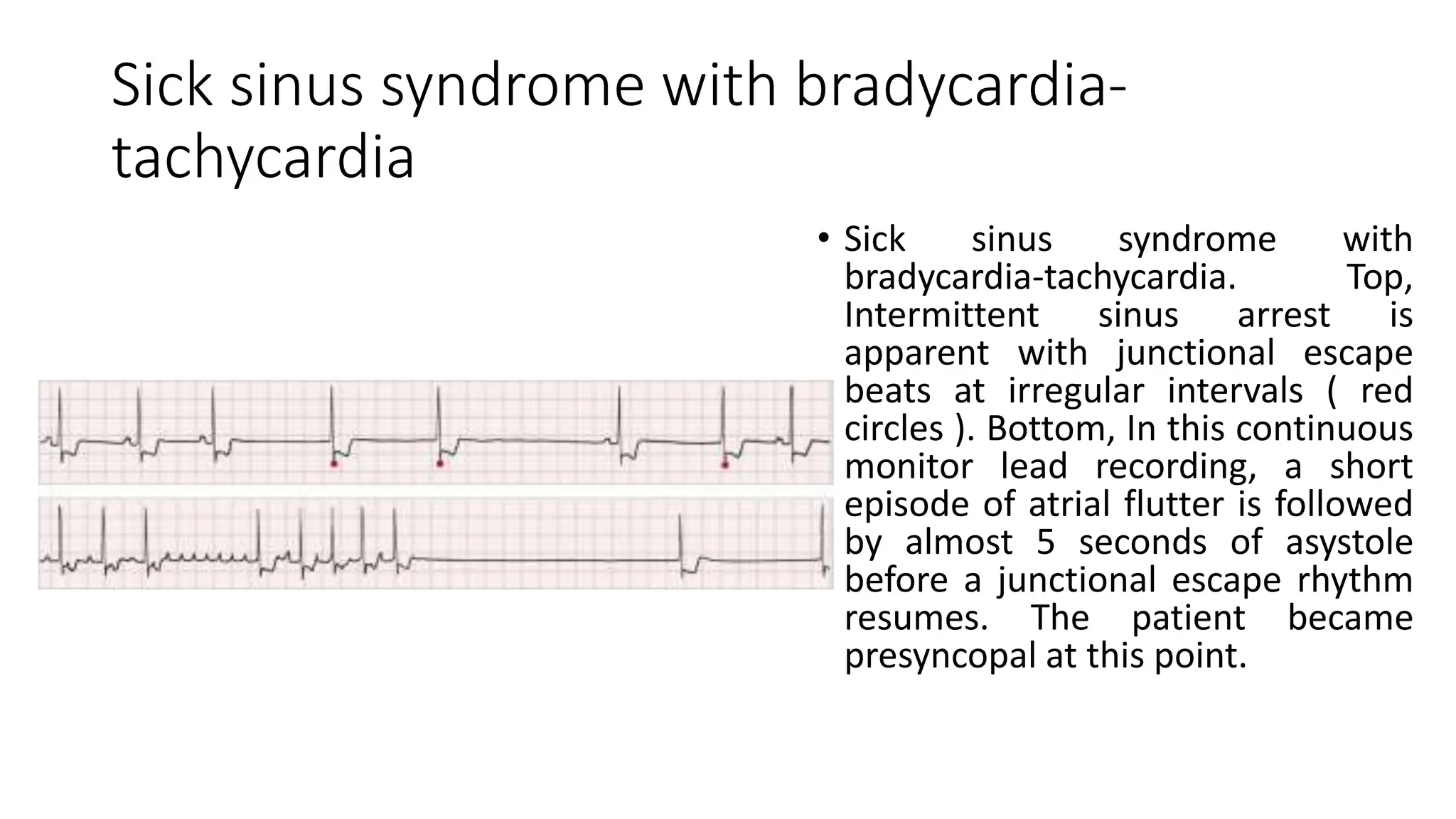
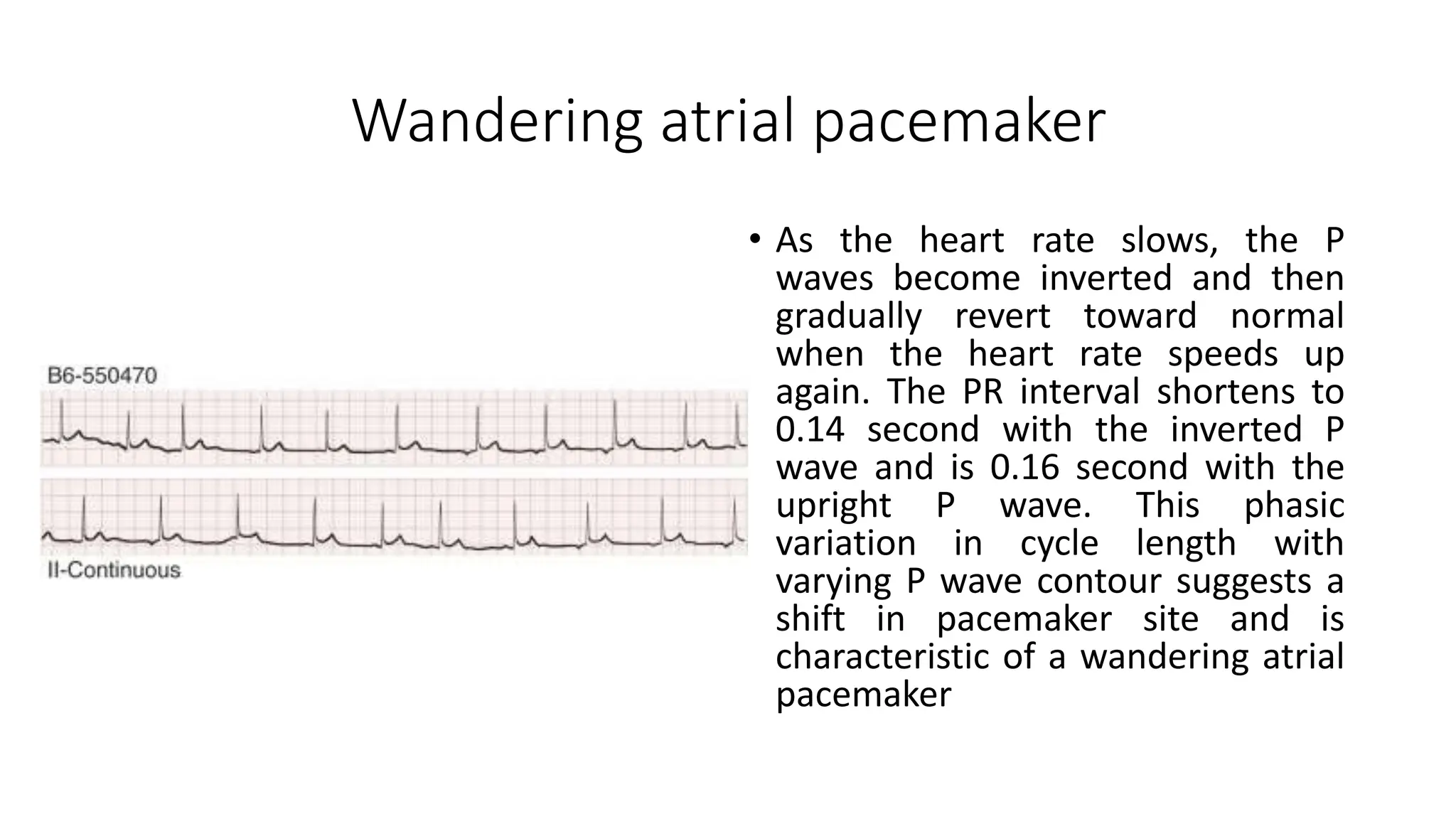
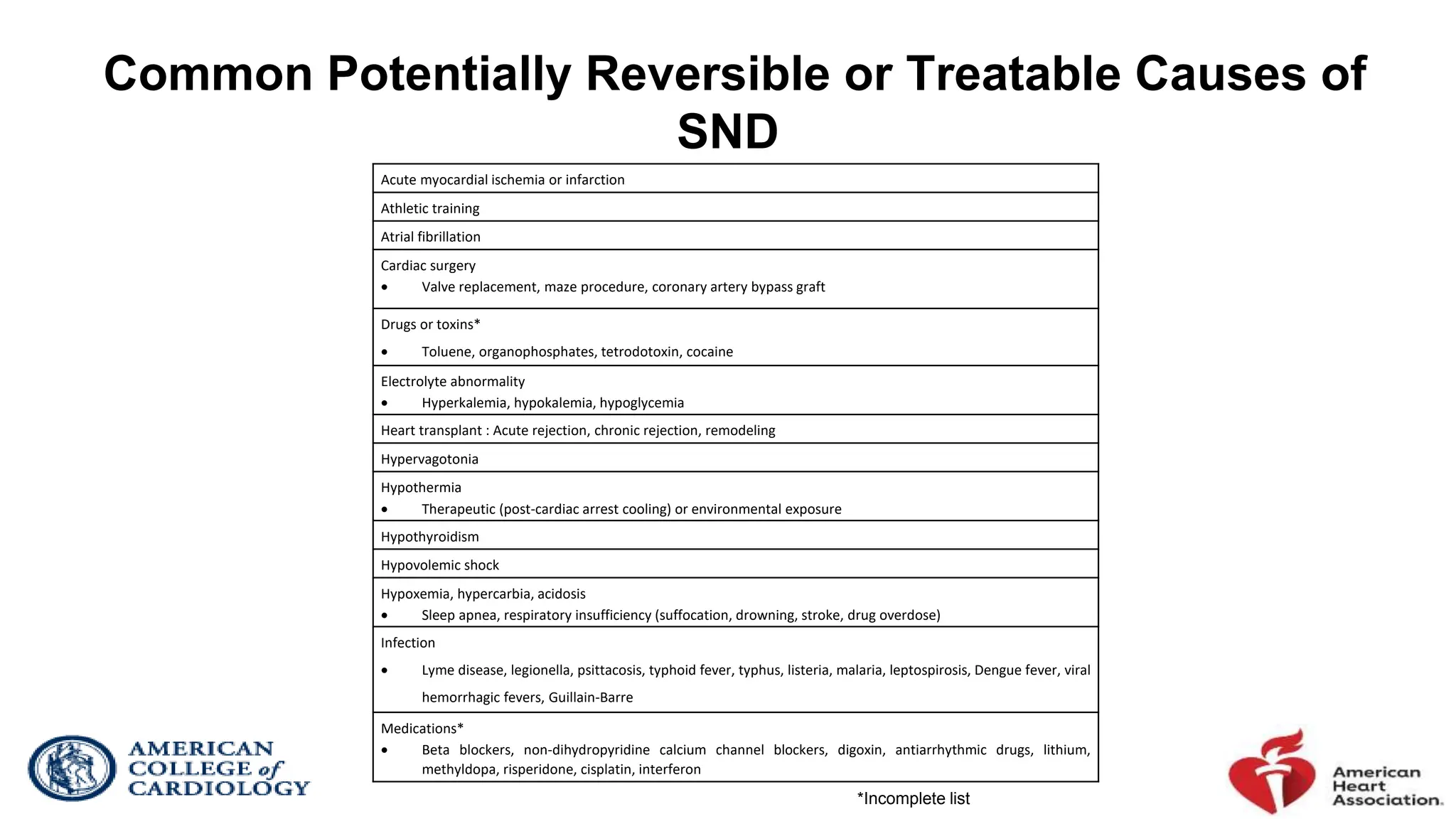
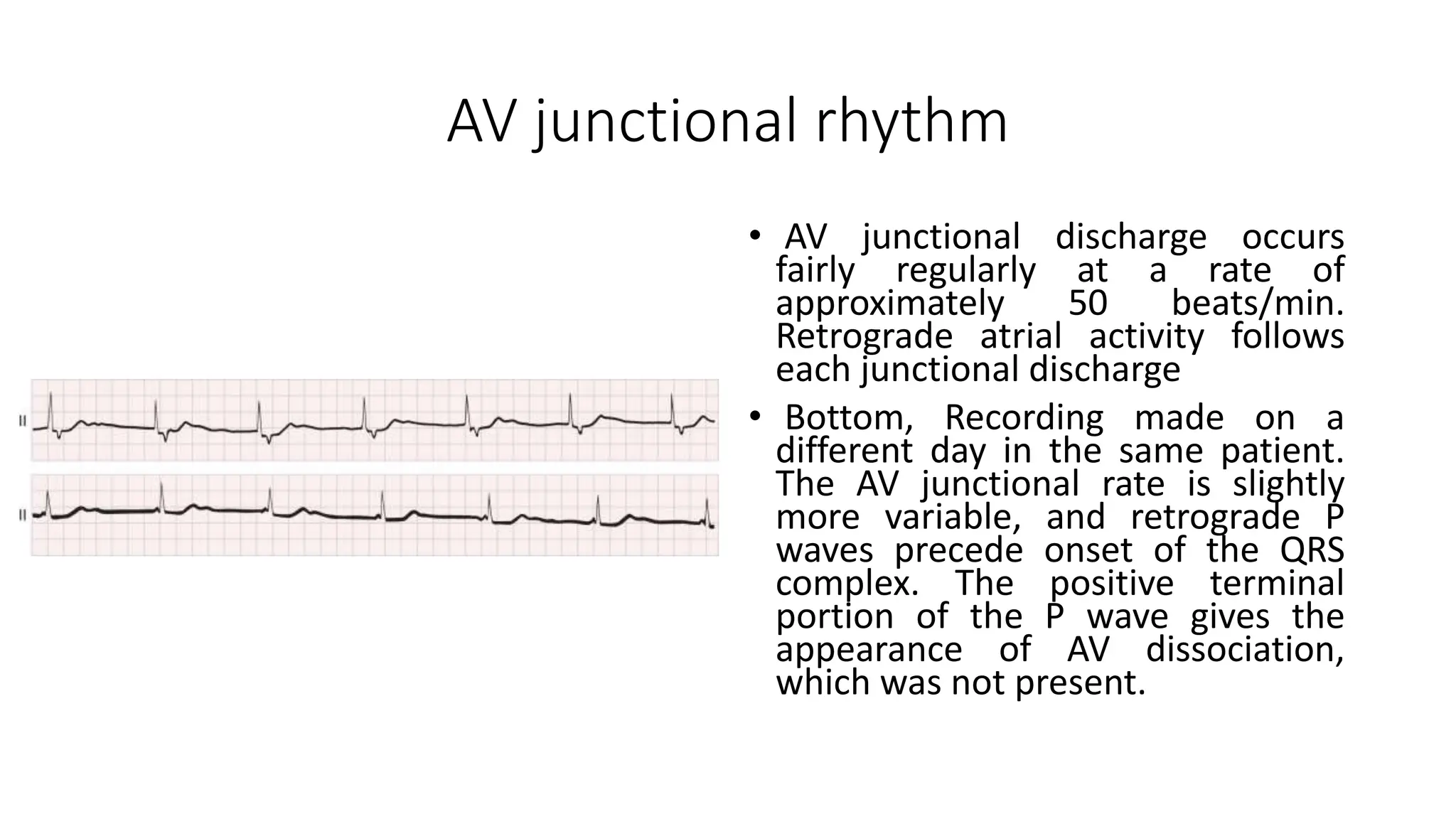
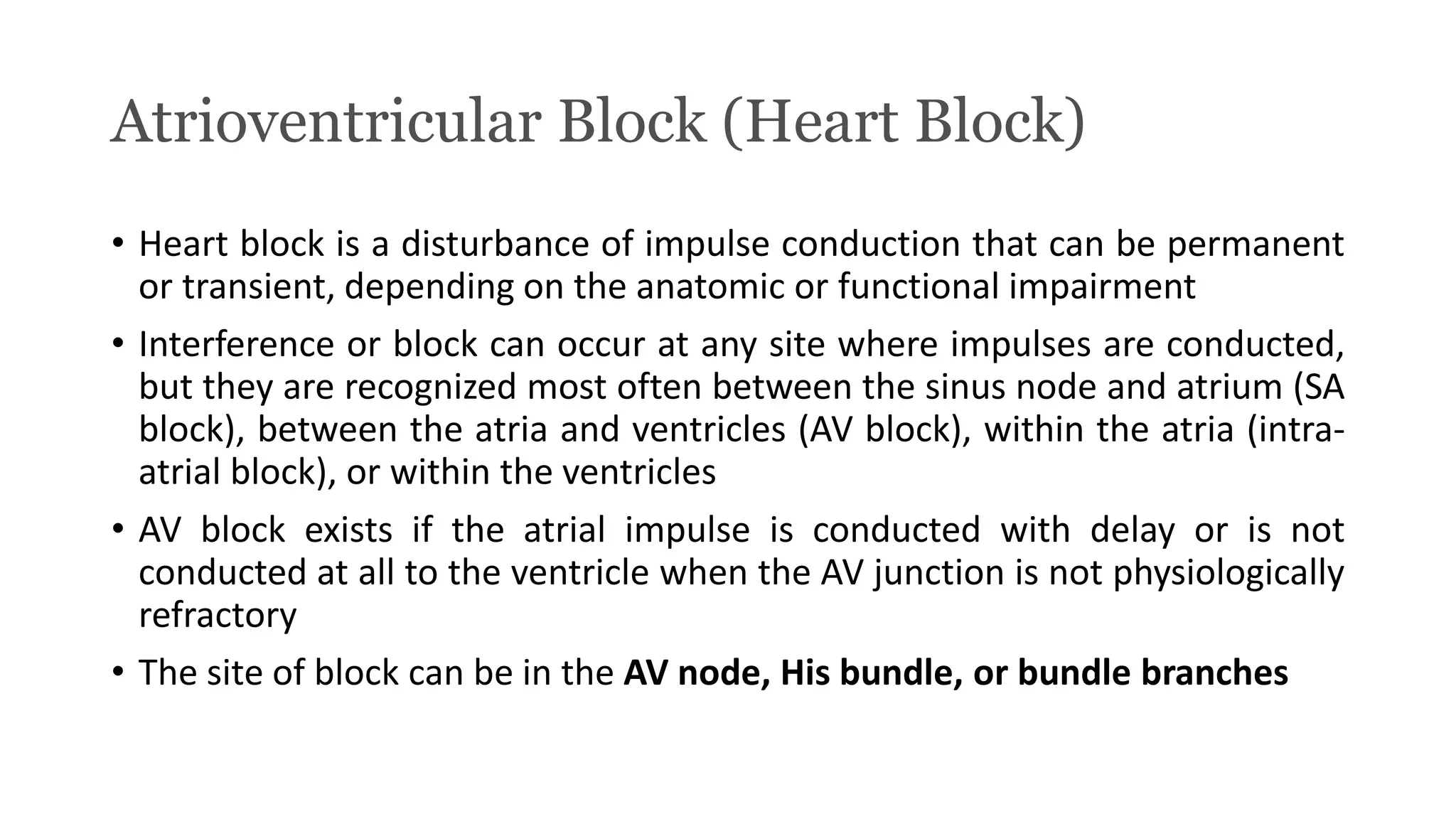
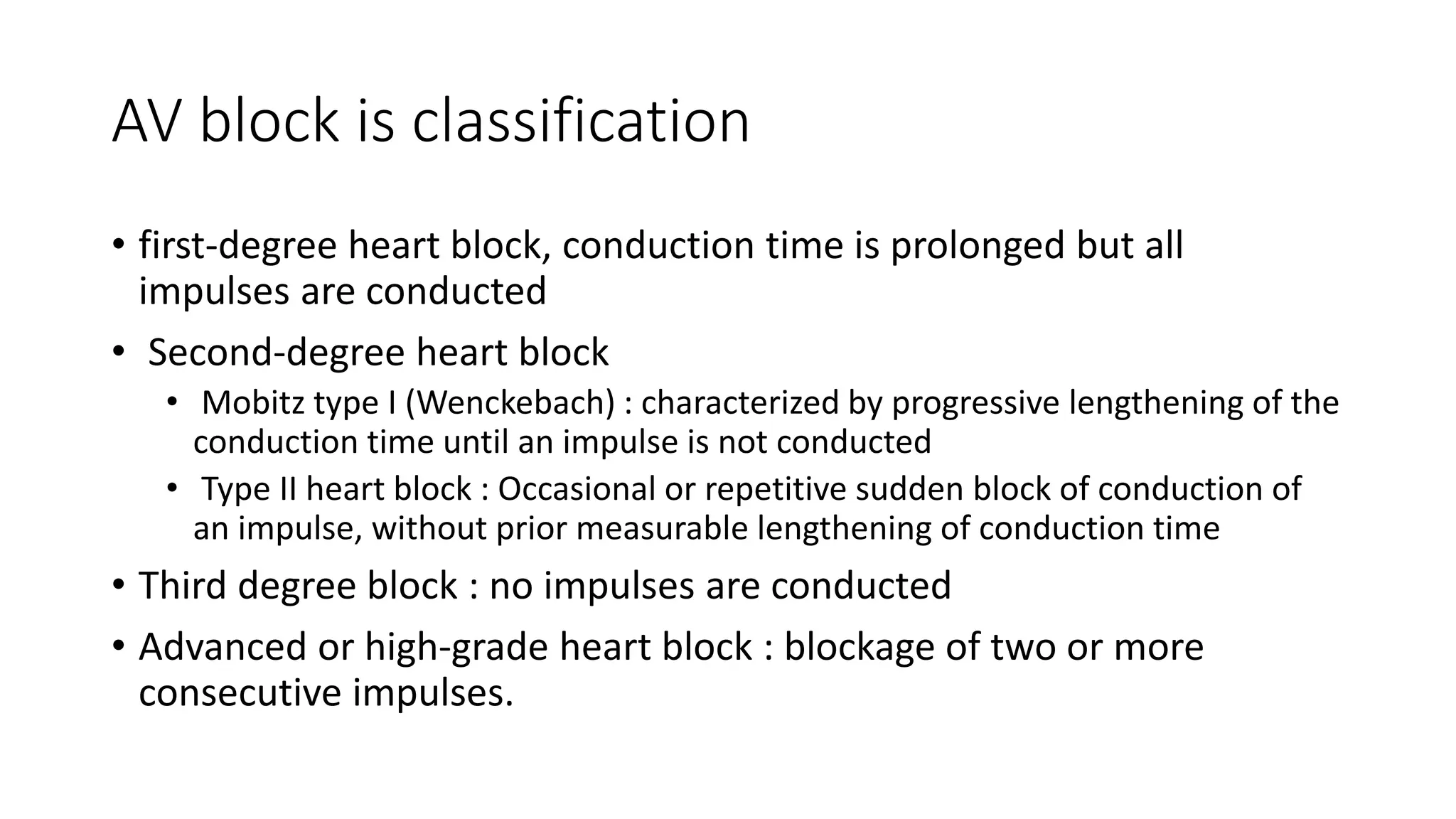
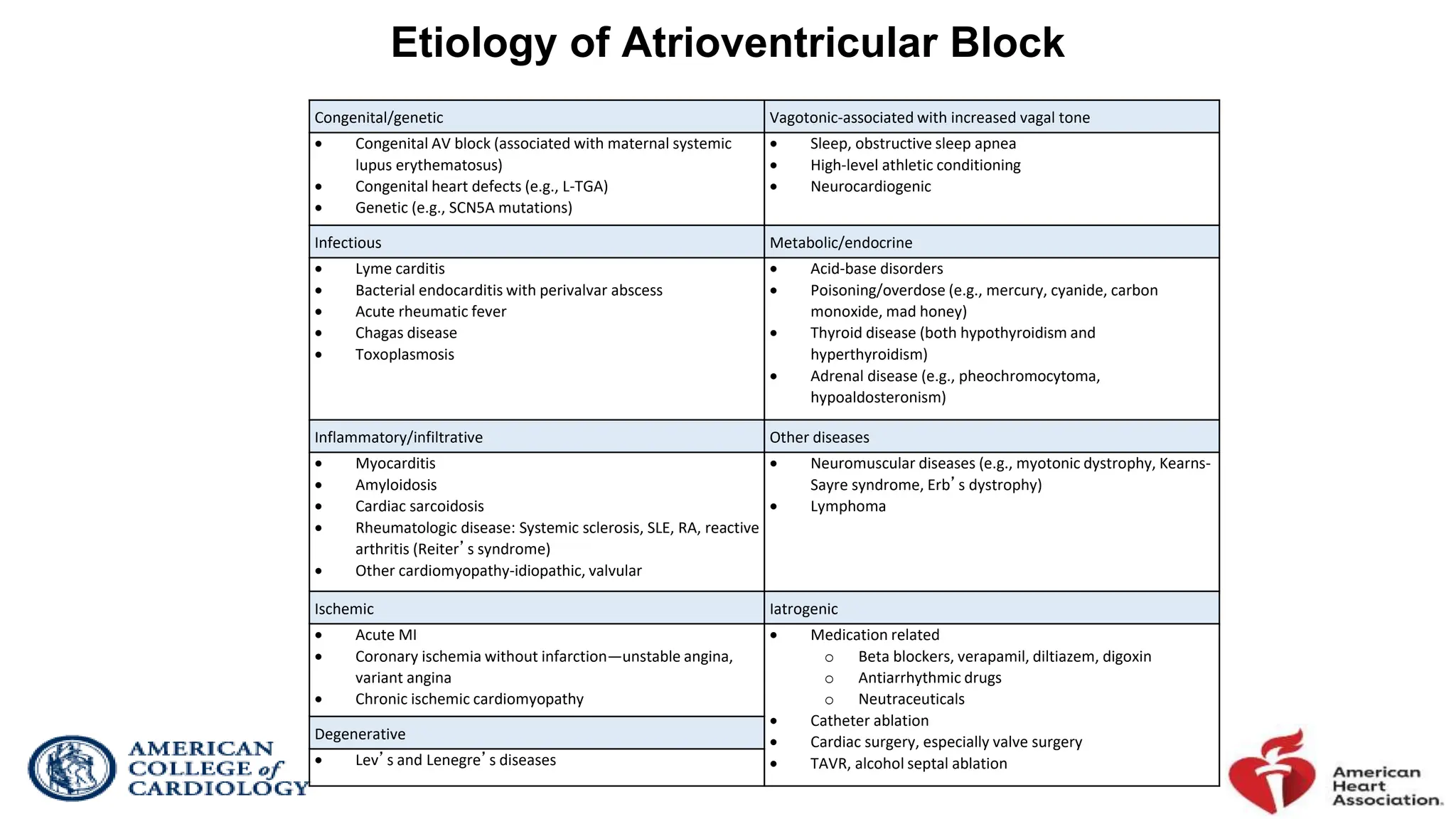
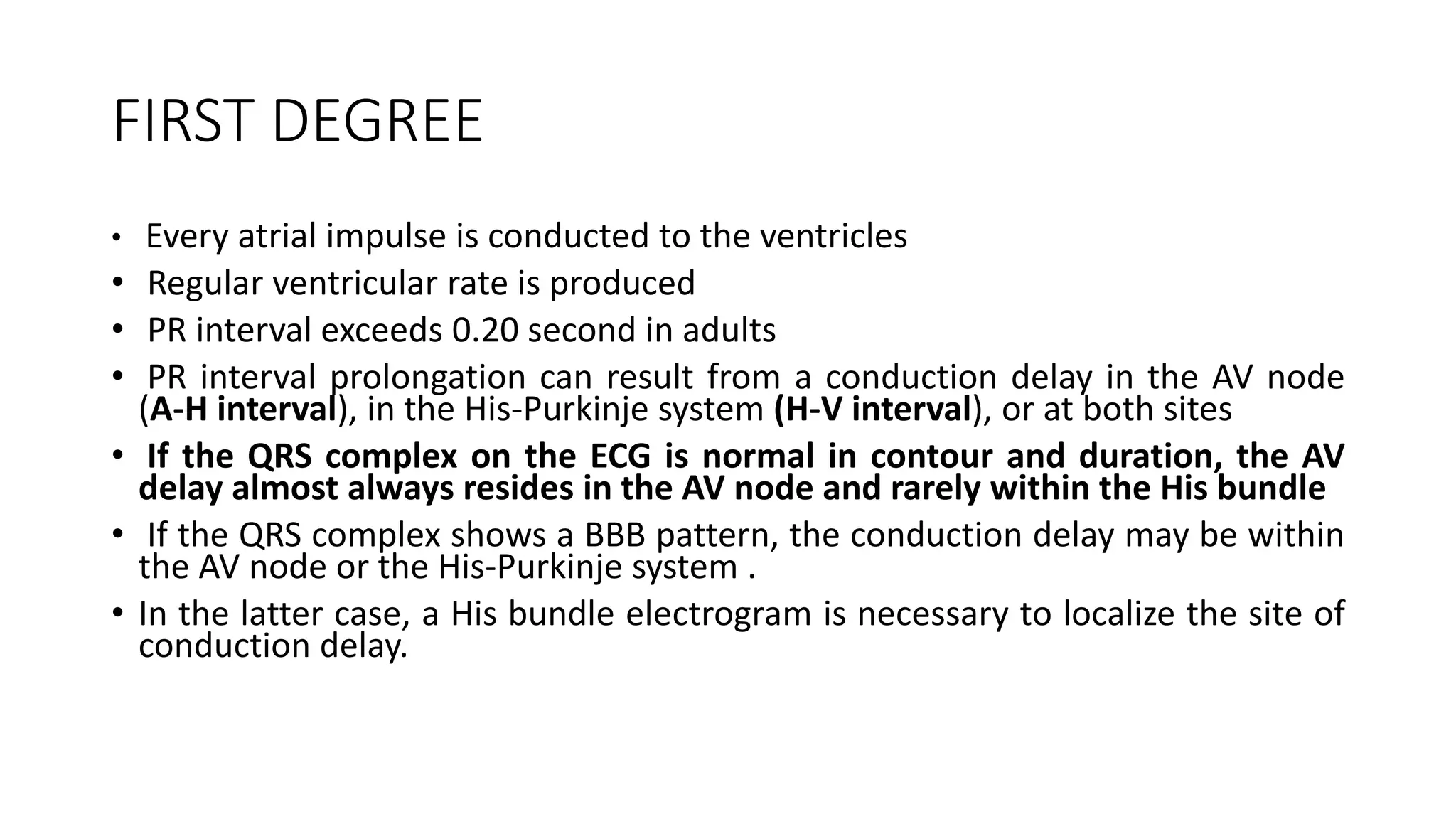
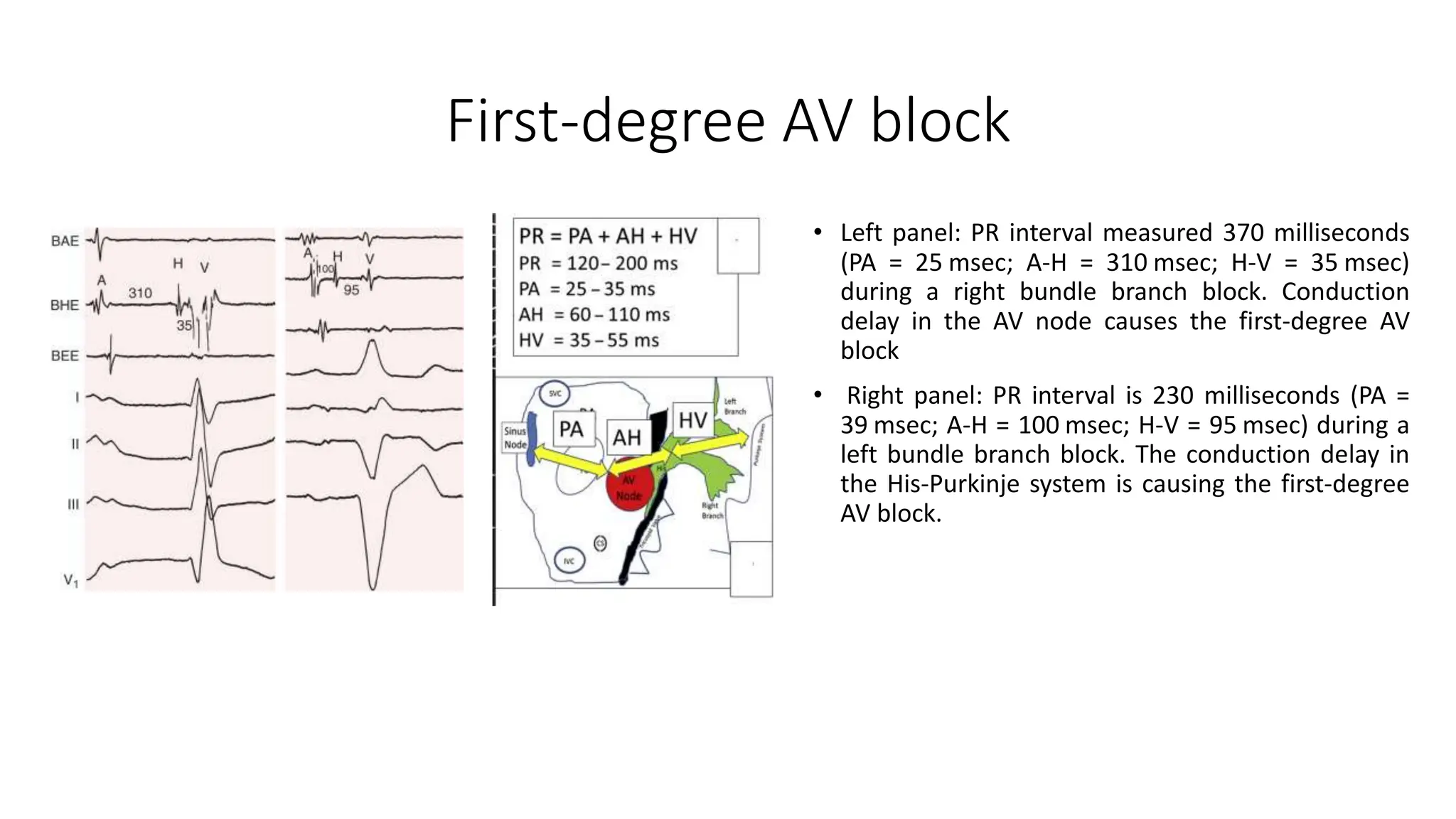
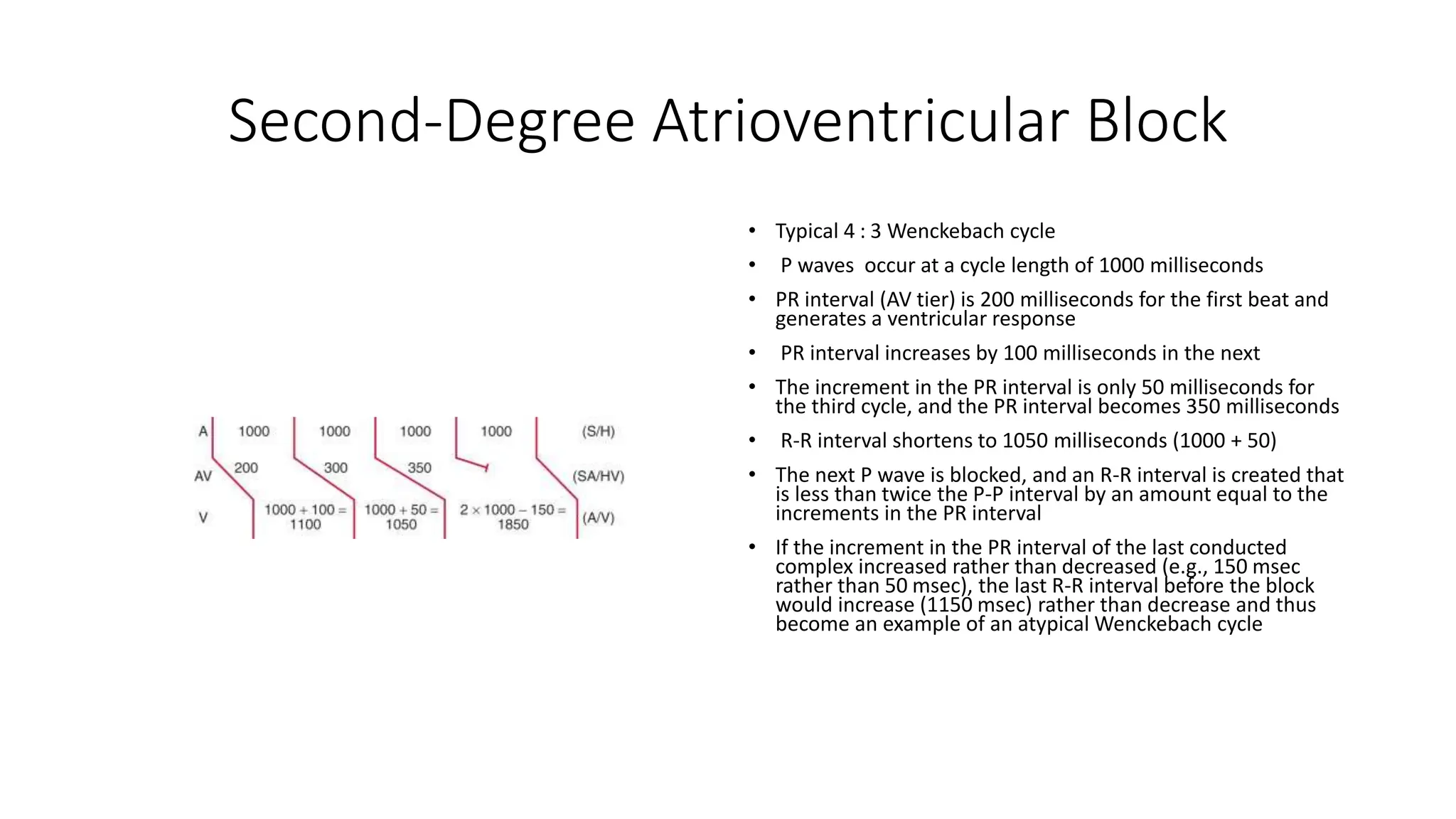
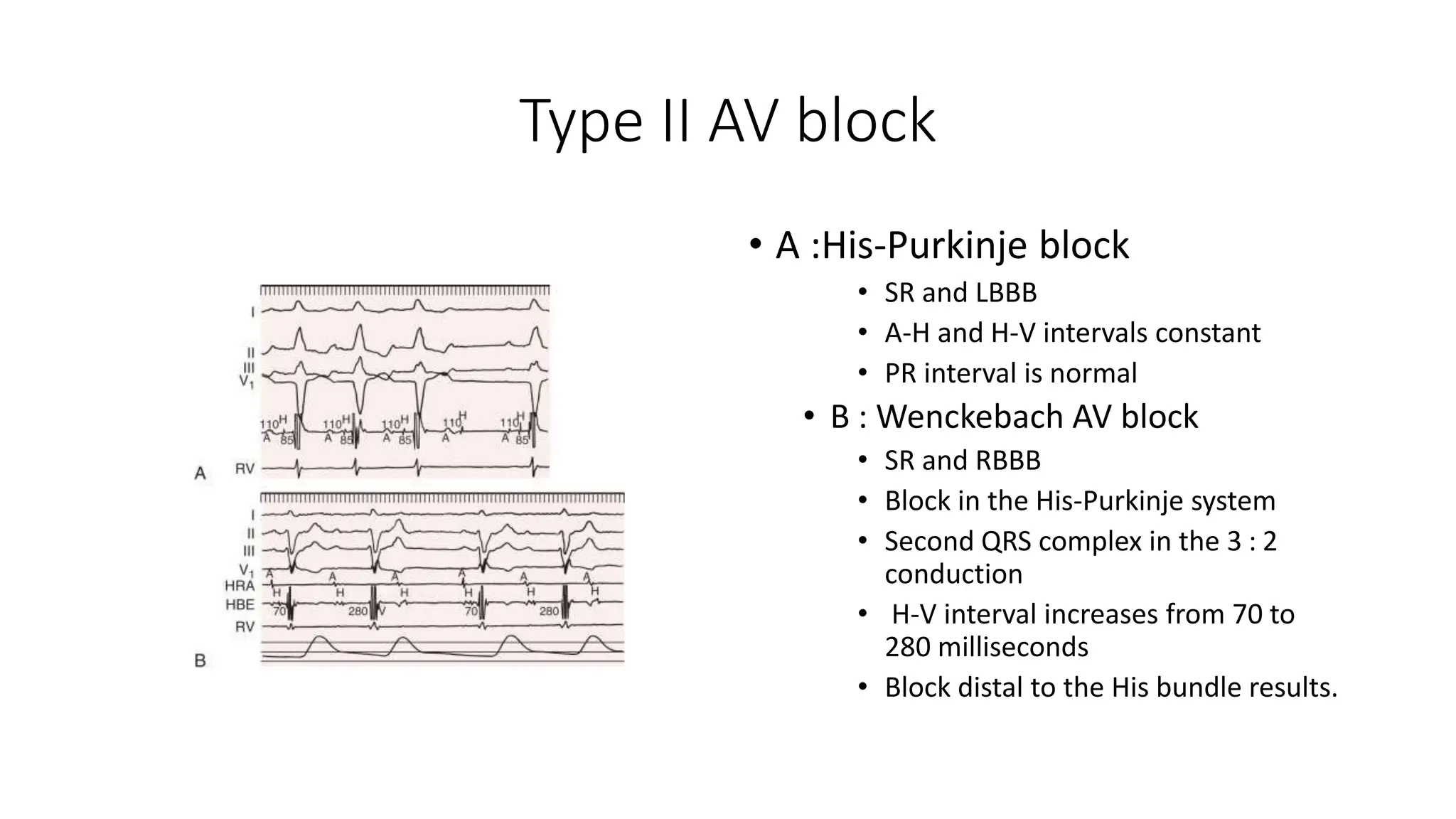
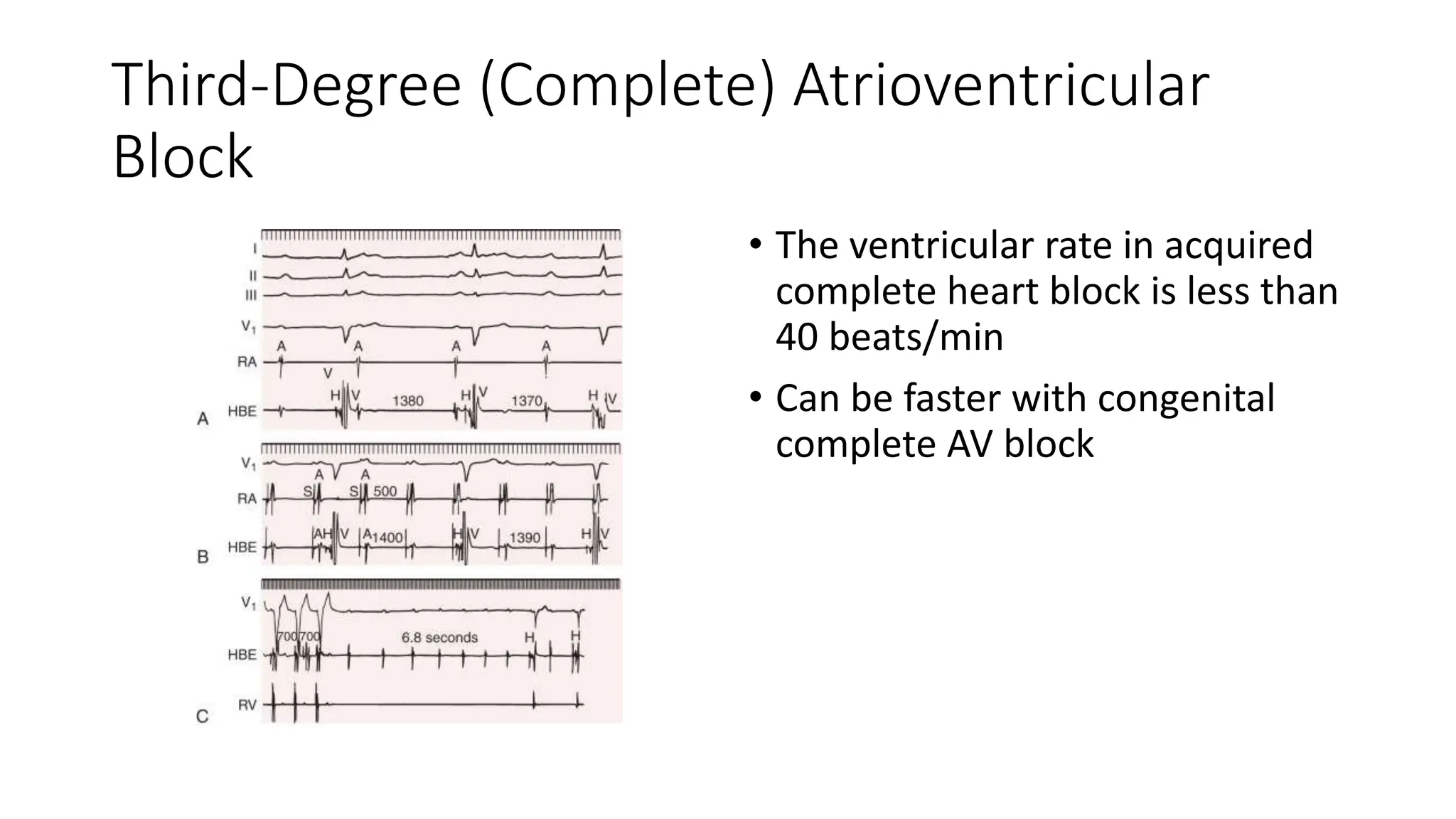
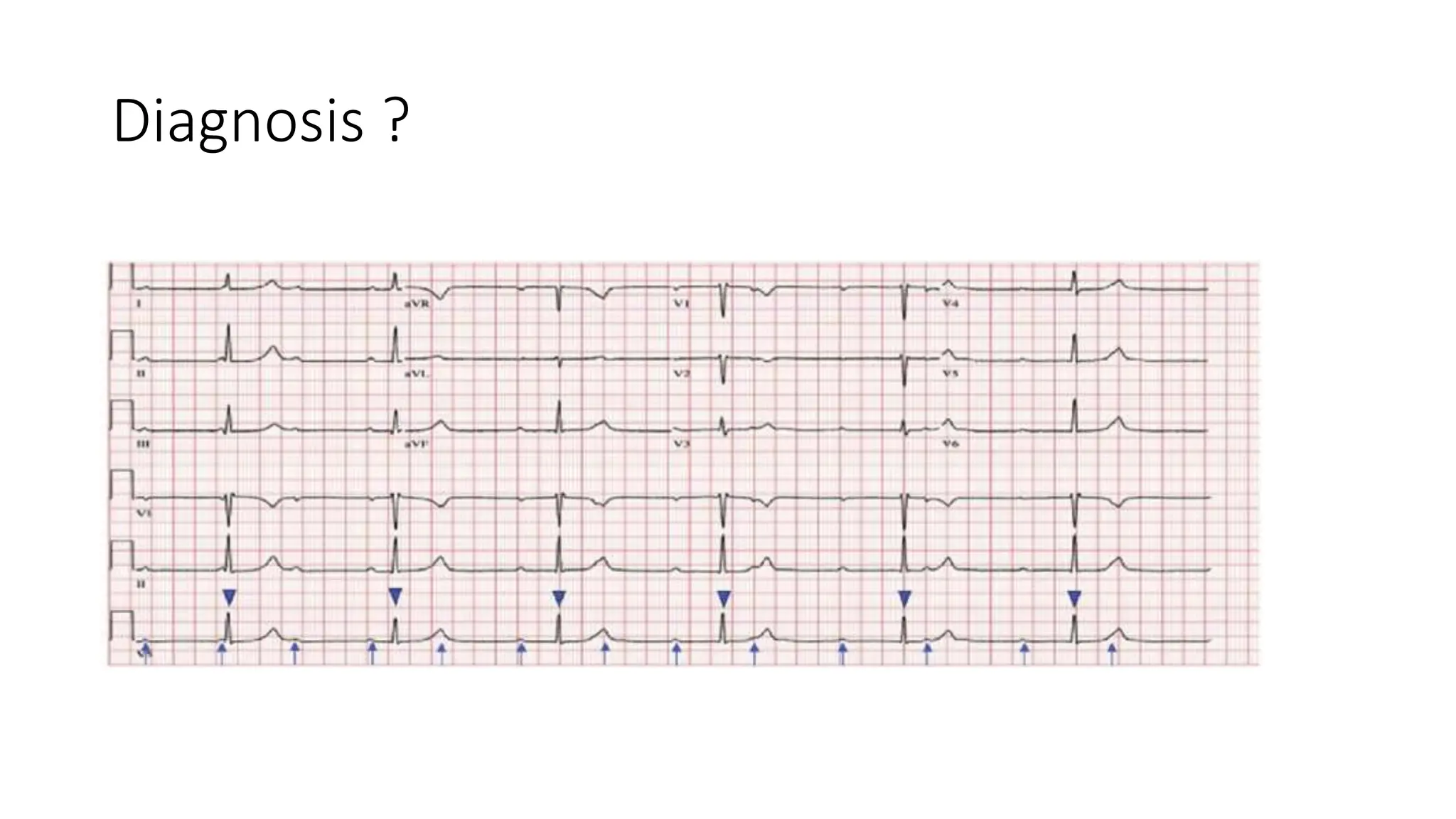
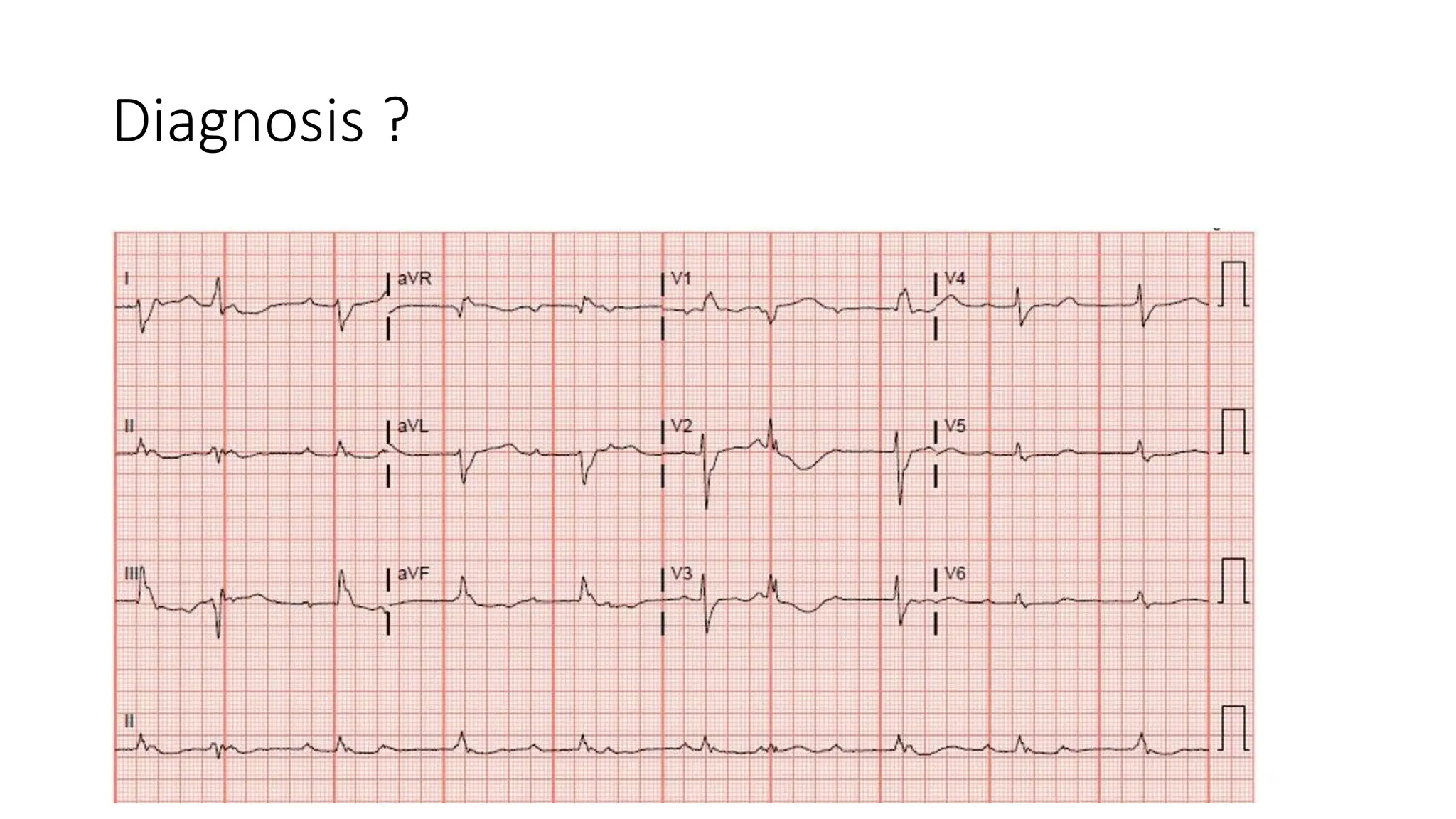
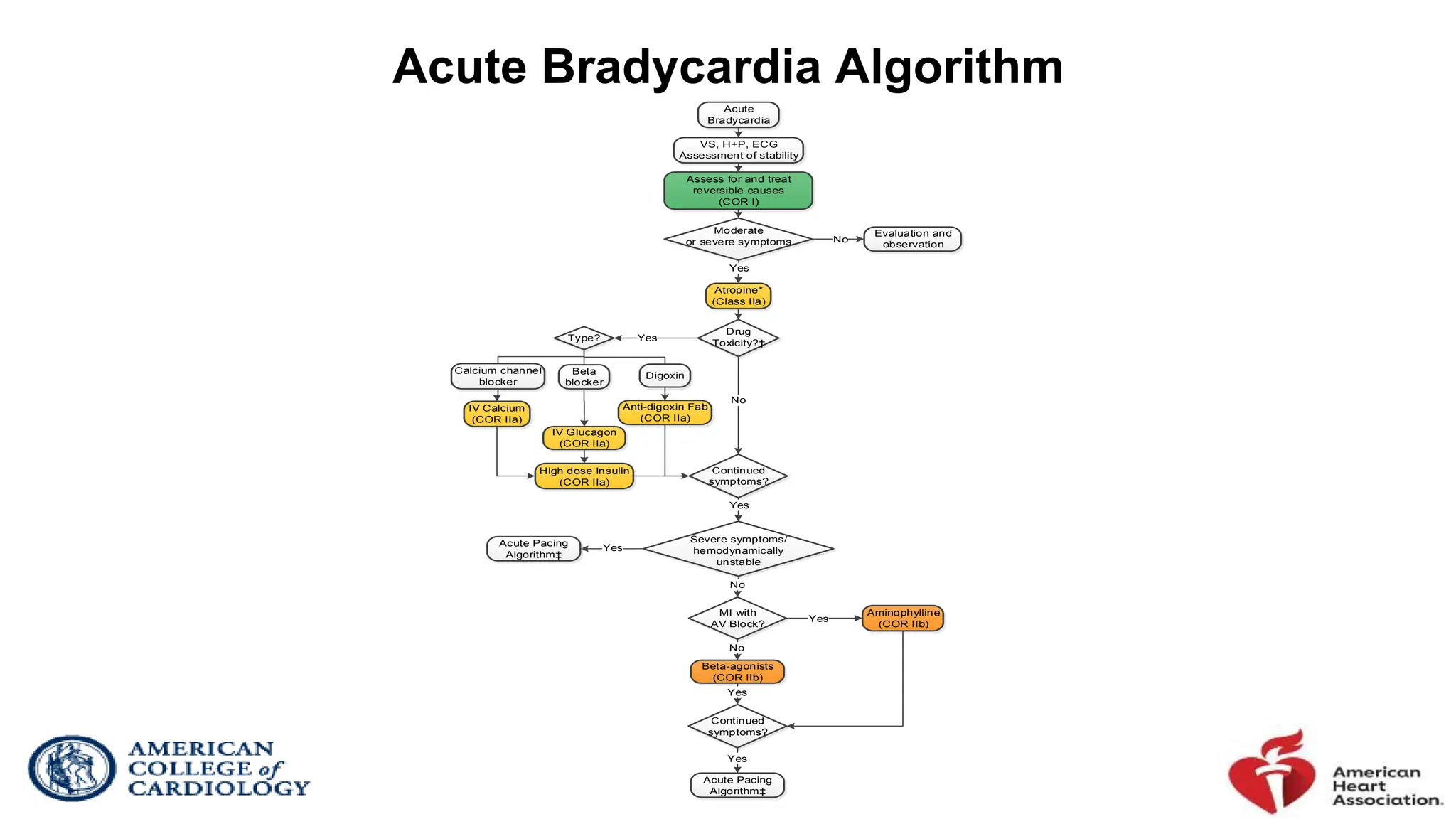
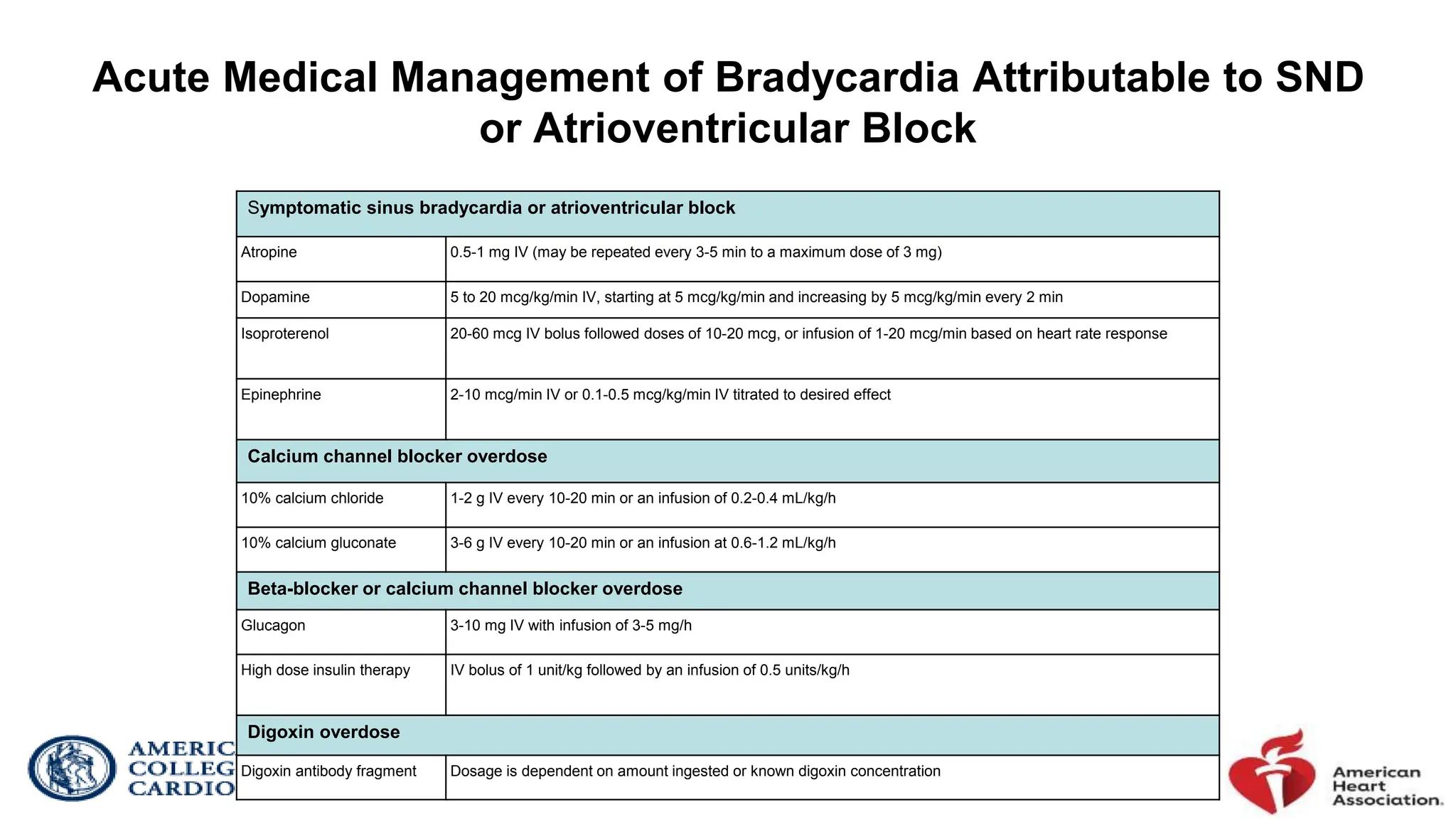
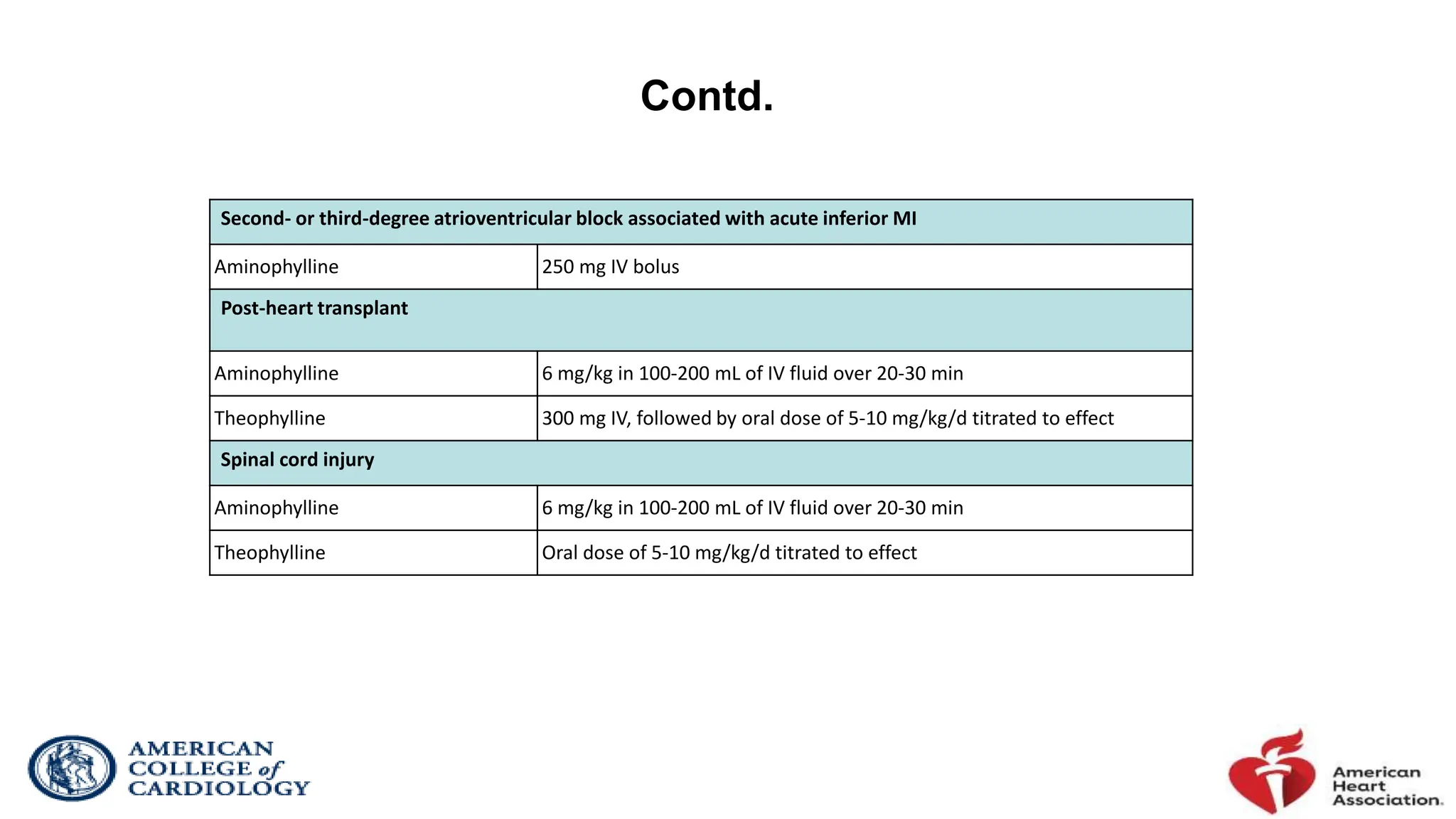
The document discusses various types of heart block and arrhythmias, including sinoatrial (SA) exit blocks and atrioventricular (AV) blocks, detailing their characteristics, causes, and diagnosis. It highlights sick sinus syndrome, bradycardia-tachycardia syndrome, and potential reversible causes of sinus node dysfunction, along with treatment algorithms for managing acute bradycardia associated with significant heart block. The information is dense and technical, aimed at providing a comprehensive understanding of cardiac conduction disorders.