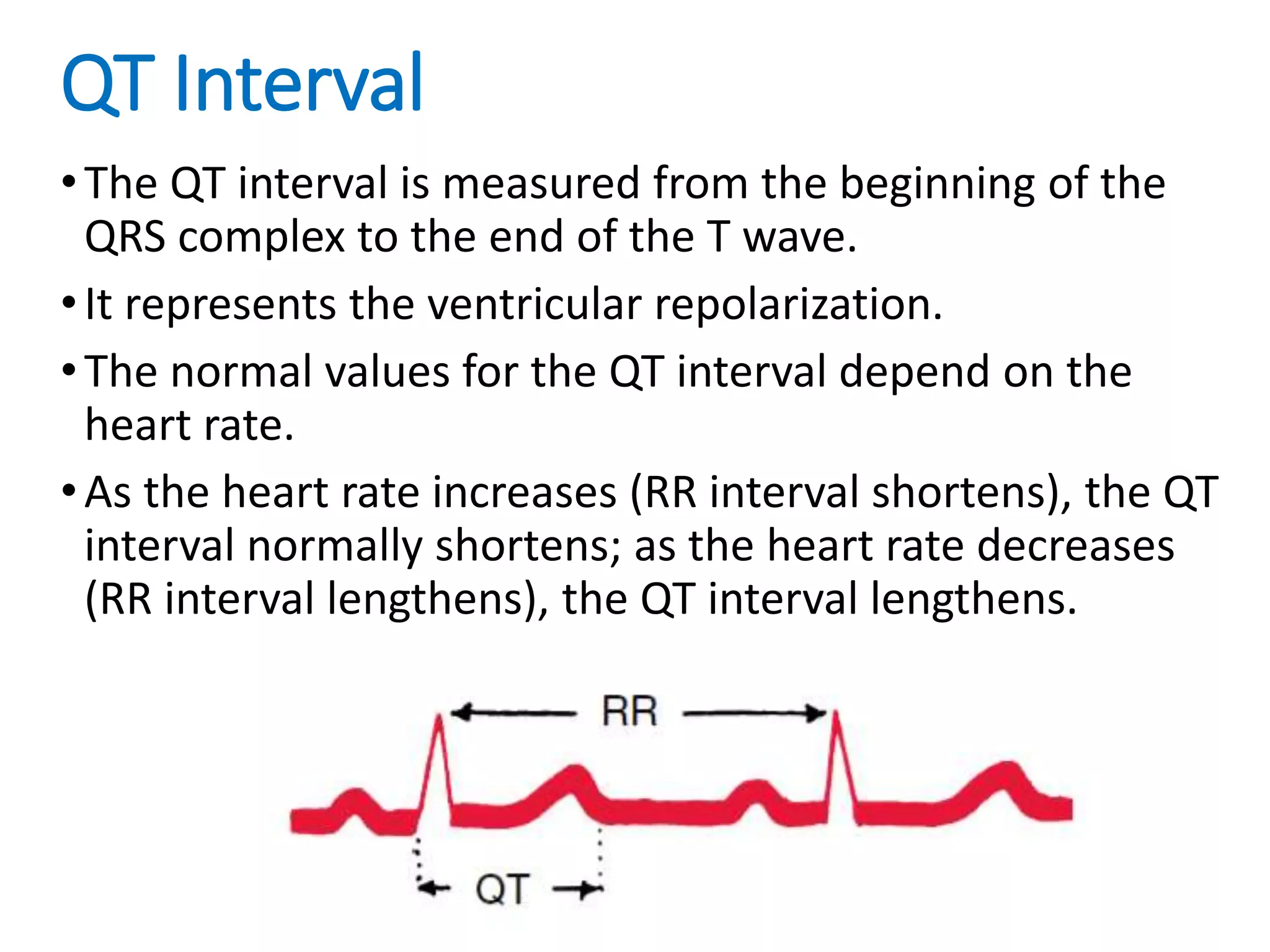
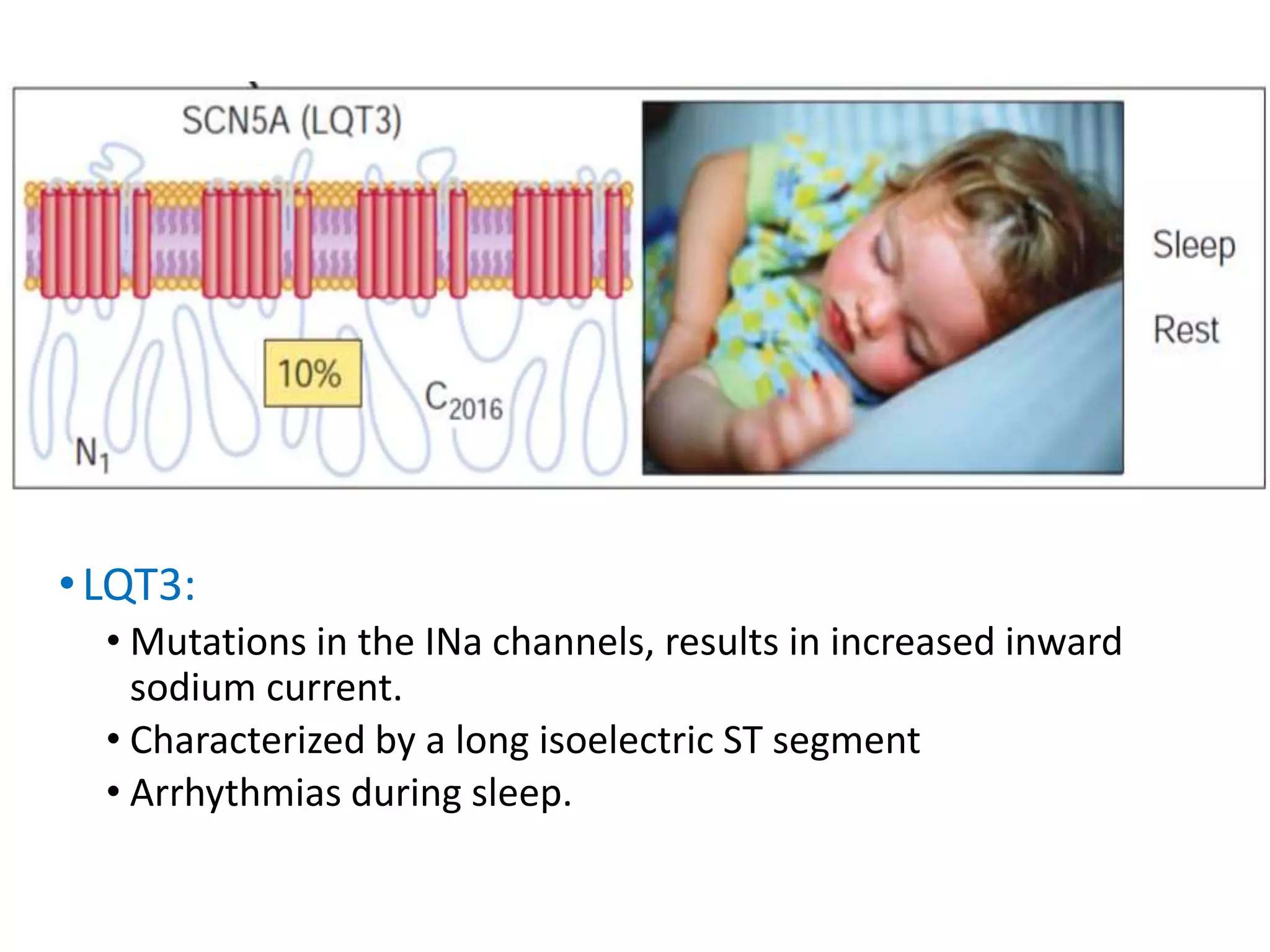
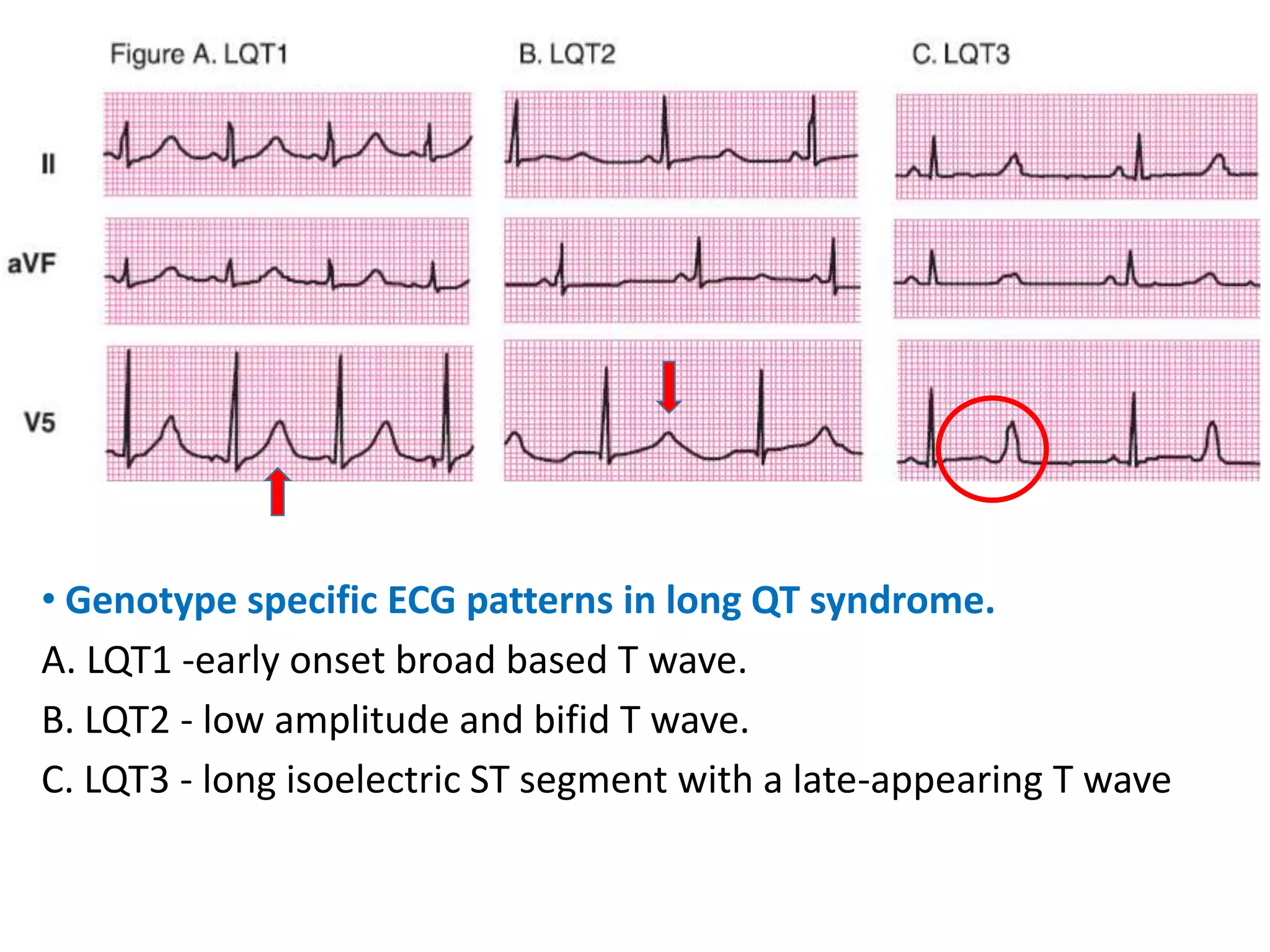
The document discusses Long QT Syndrome (LQTS), an inherited heart condition characterized by an abnormally prolonged QT interval on electrocardiograms. It describes the causes and types of LQTS, including LQT1, LQT2 and LQT3, which are associated with different genetic mutations and ECG patterns. The main symptoms of LQTS are syncope and cardiac arrest, typically in children or teenagers. Diagnosis involves measuring the QT interval and identifying risk factors. Treatment focuses on beta-blockers, lifestyle changes and implantable cardioverter-defibrillators for high-risk patients.