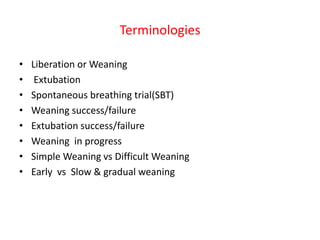
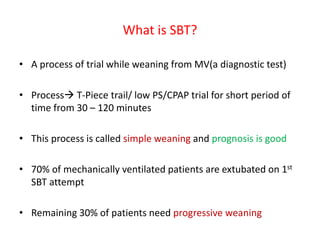
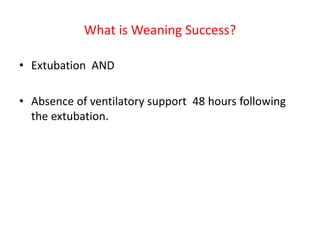
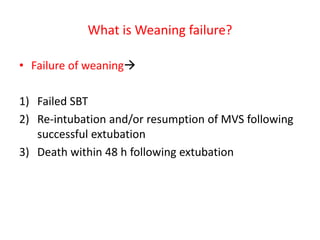
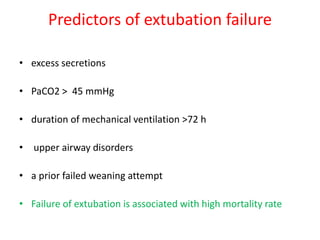
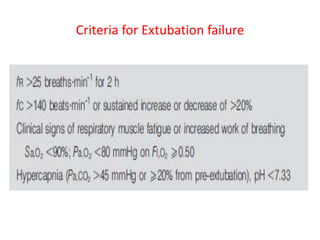
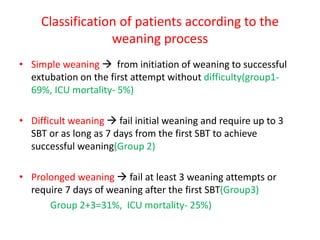
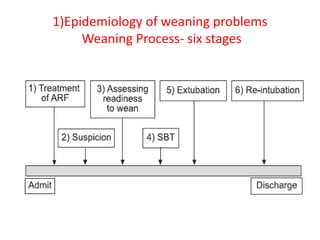
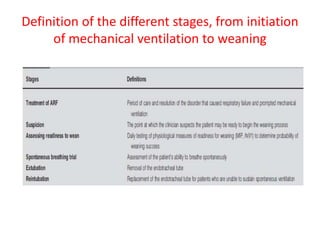
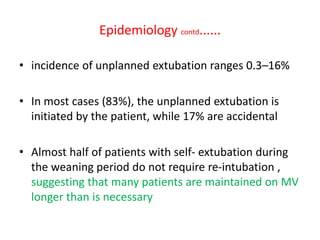
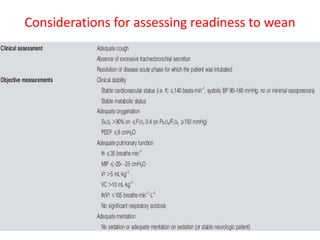
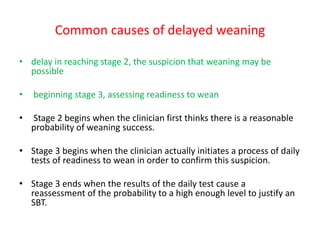
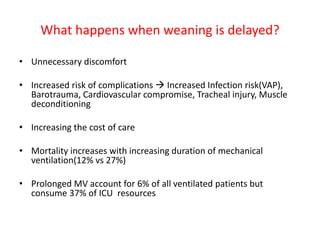
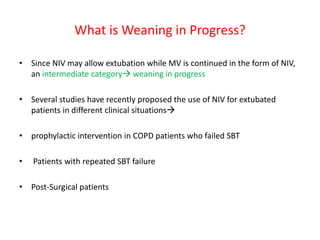
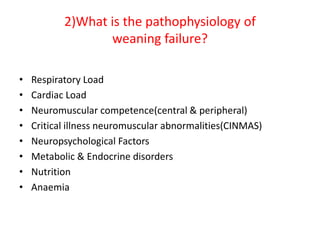
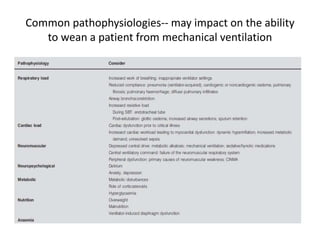
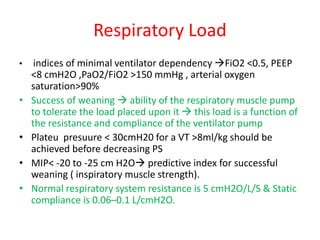
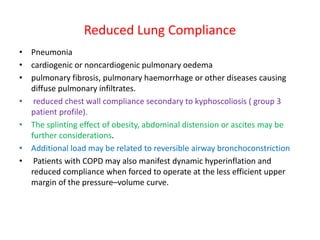
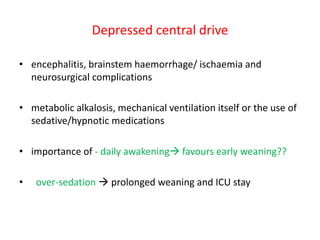
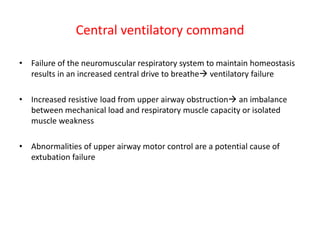
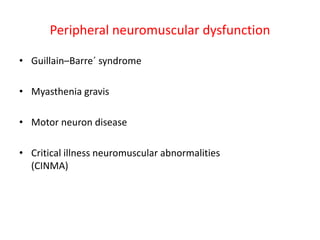
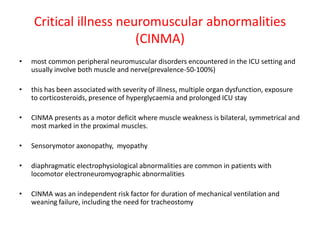
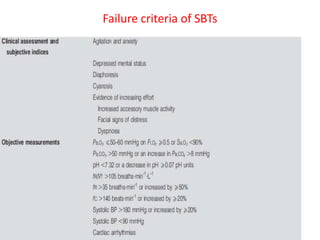
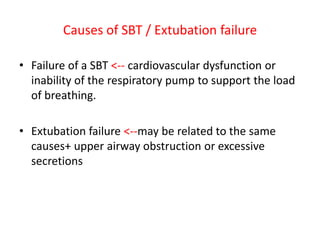
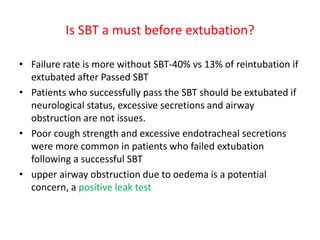
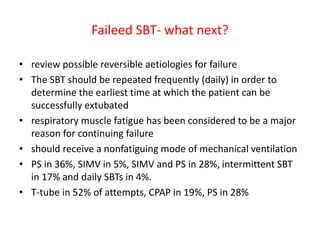
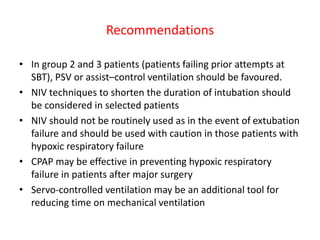
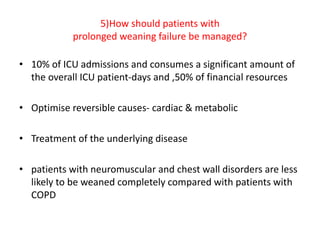
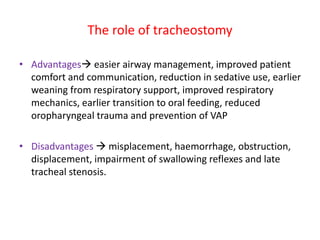
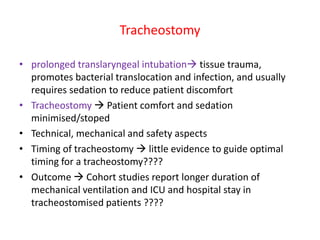
This document discusses weaning from mechanical ventilation. It defines key terms like liberation, extubation, spontaneous breathing trials (SBT), and weaning success and failure. It describes the process of conducting an SBT to assess readiness for extubation. Factors that can lead to weaning failure like respiratory load, cardiac load, neuromuscular issues, and psychological factors are reviewed. Finally, it discusses using different ventilator modes like pressure support ventilation to aid in more difficult weaning cases.