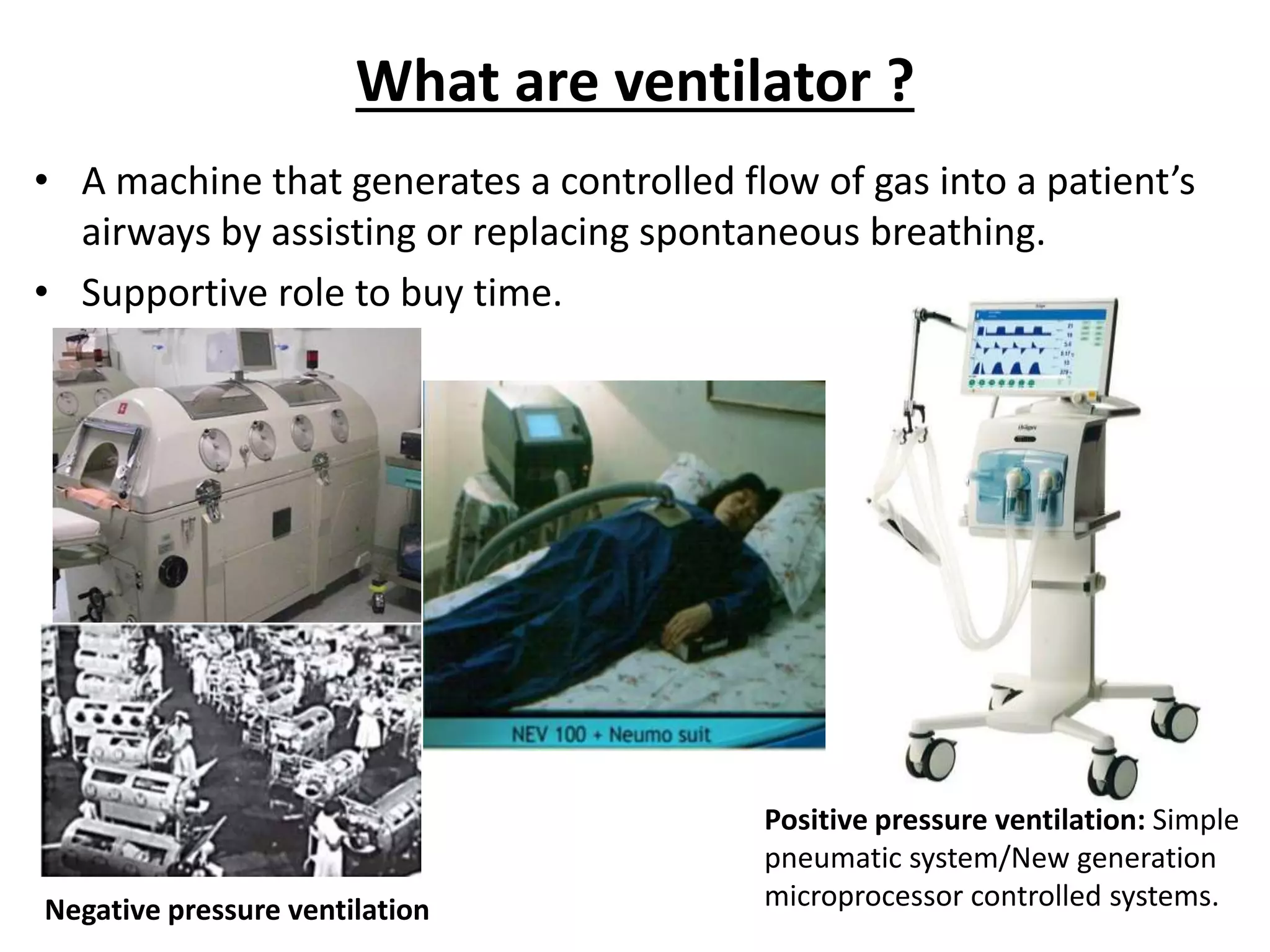
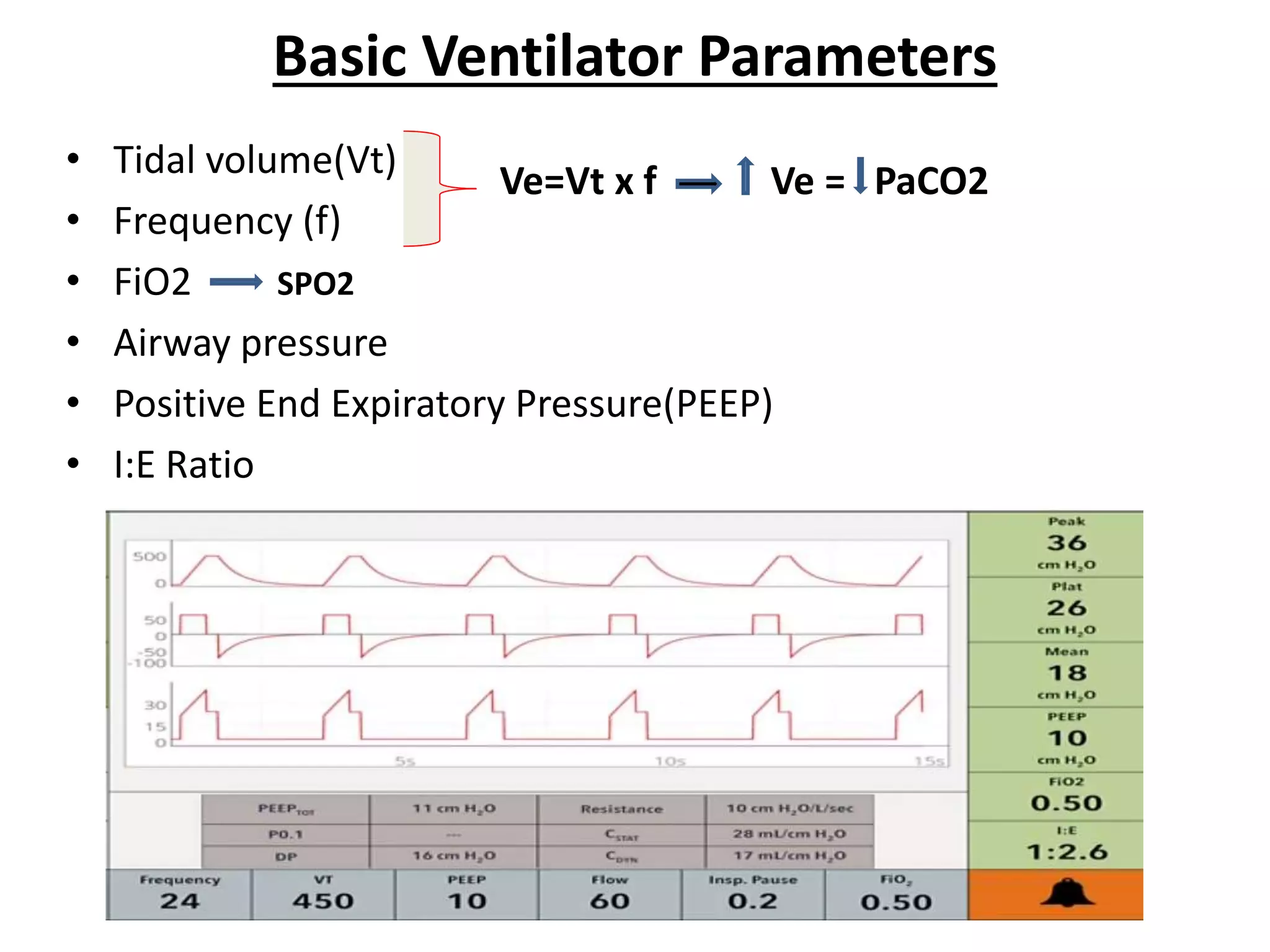
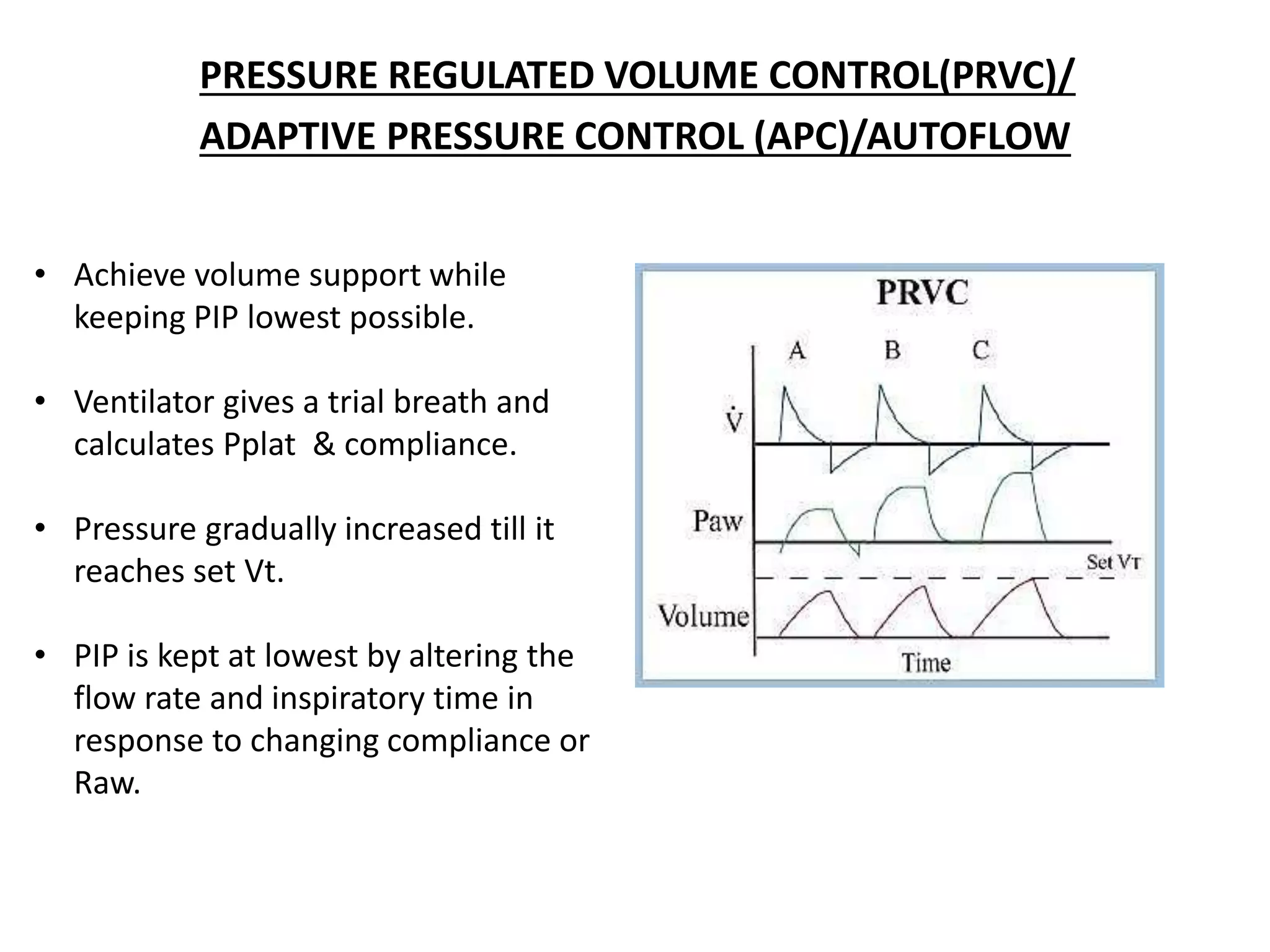
Mechanical ventilation provides positive pressure ventilation to support patients who are unable to breathe adequately on their own. The document discusses various modes of mechanical ventilation including controlled mandatory ventilation, volume control ventilation, pressure control ventilation, assisted-control ventilation, synchronized intermittent mandatory ventilation, and pressure support ventilation. It explains the basic parameters used in mechanical ventilation like tidal volume, respiratory rate, PEEP, and I:E ratio. It also discusses principles of weaning a patient from mechanical ventilation and assessing readiness for weaning.