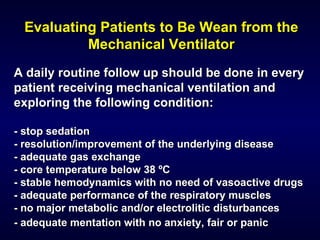
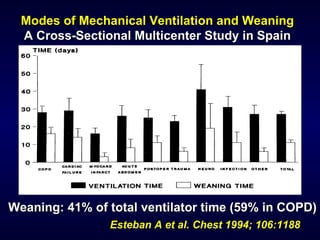
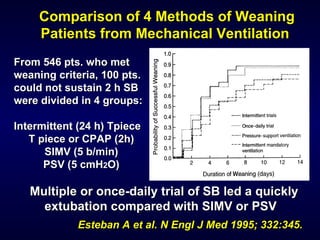
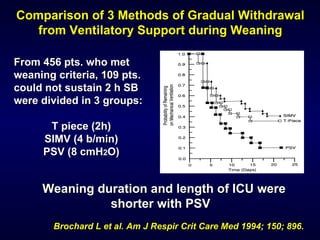
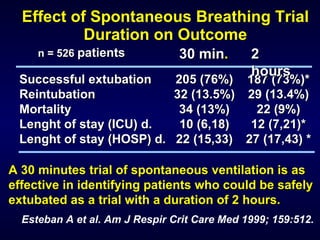
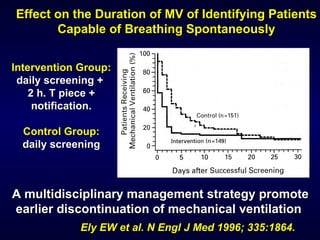
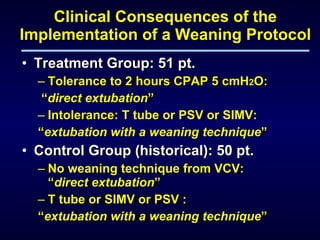
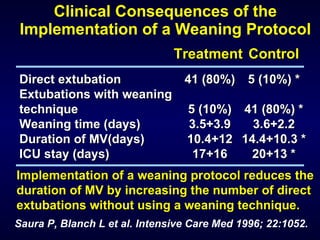
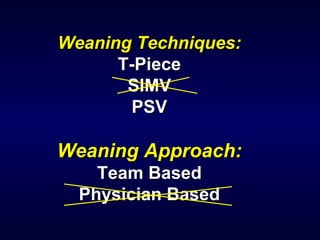
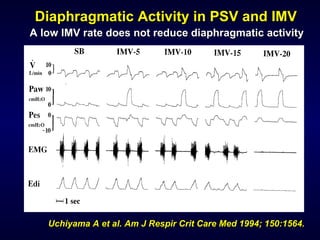
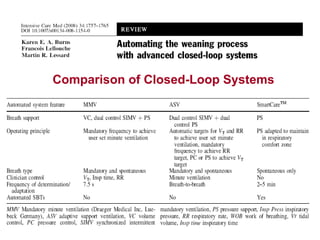
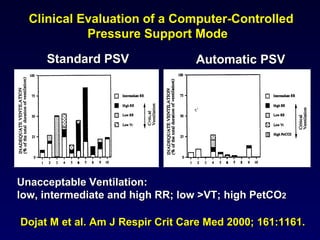
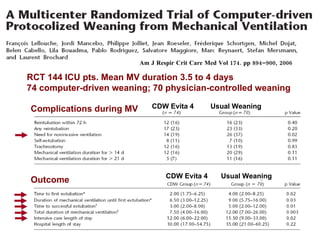
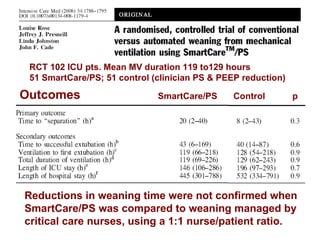
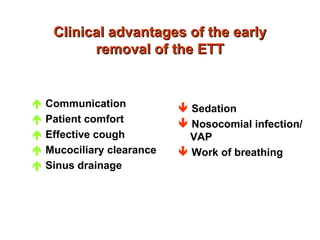
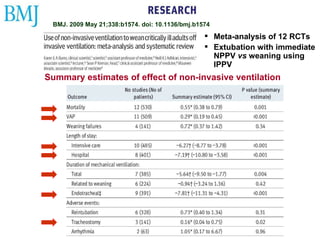
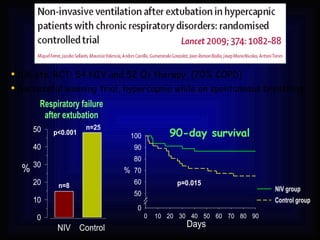
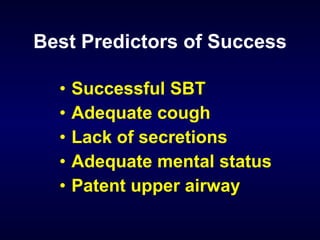
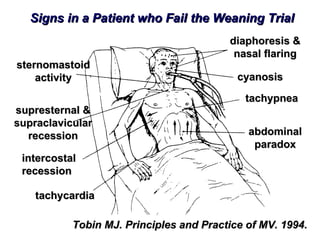
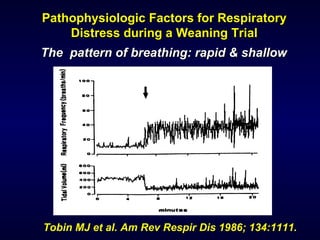
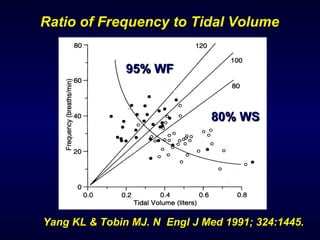
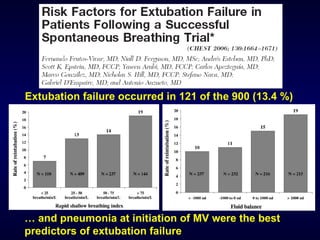
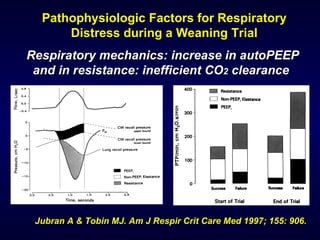
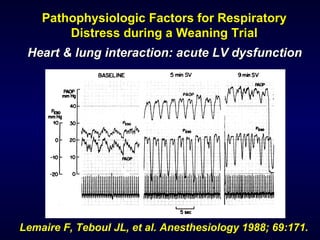
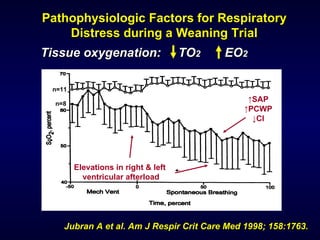
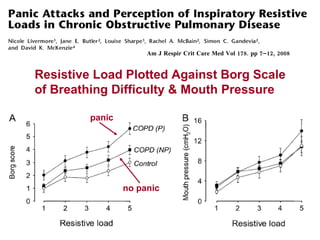
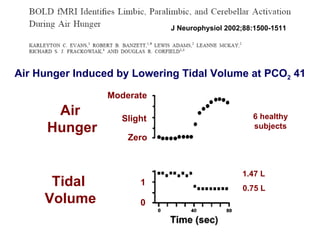
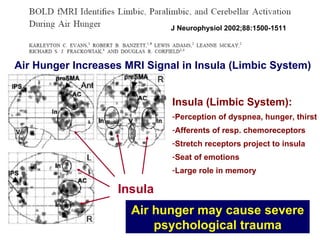
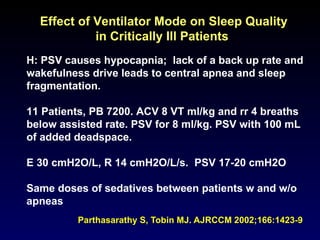
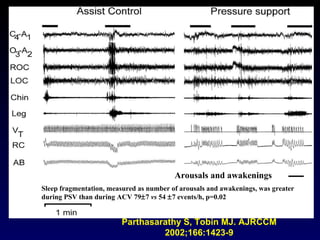
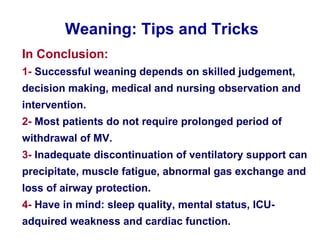
The document outlines critical care practices for weaning patients from mechanical ventilation, emphasizing the importance of daily evaluations and a multidisciplinary approach. It reviews various weaning techniques, success rates, and factors influencing weaning outcomes, and highlights the significance of psychological aspects and patient comfort during the process. Key findings suggest that shorter weaning trials can be effective and that implementation of structured weaning protocols can reduce ventilator duration and improve patient outcomes.