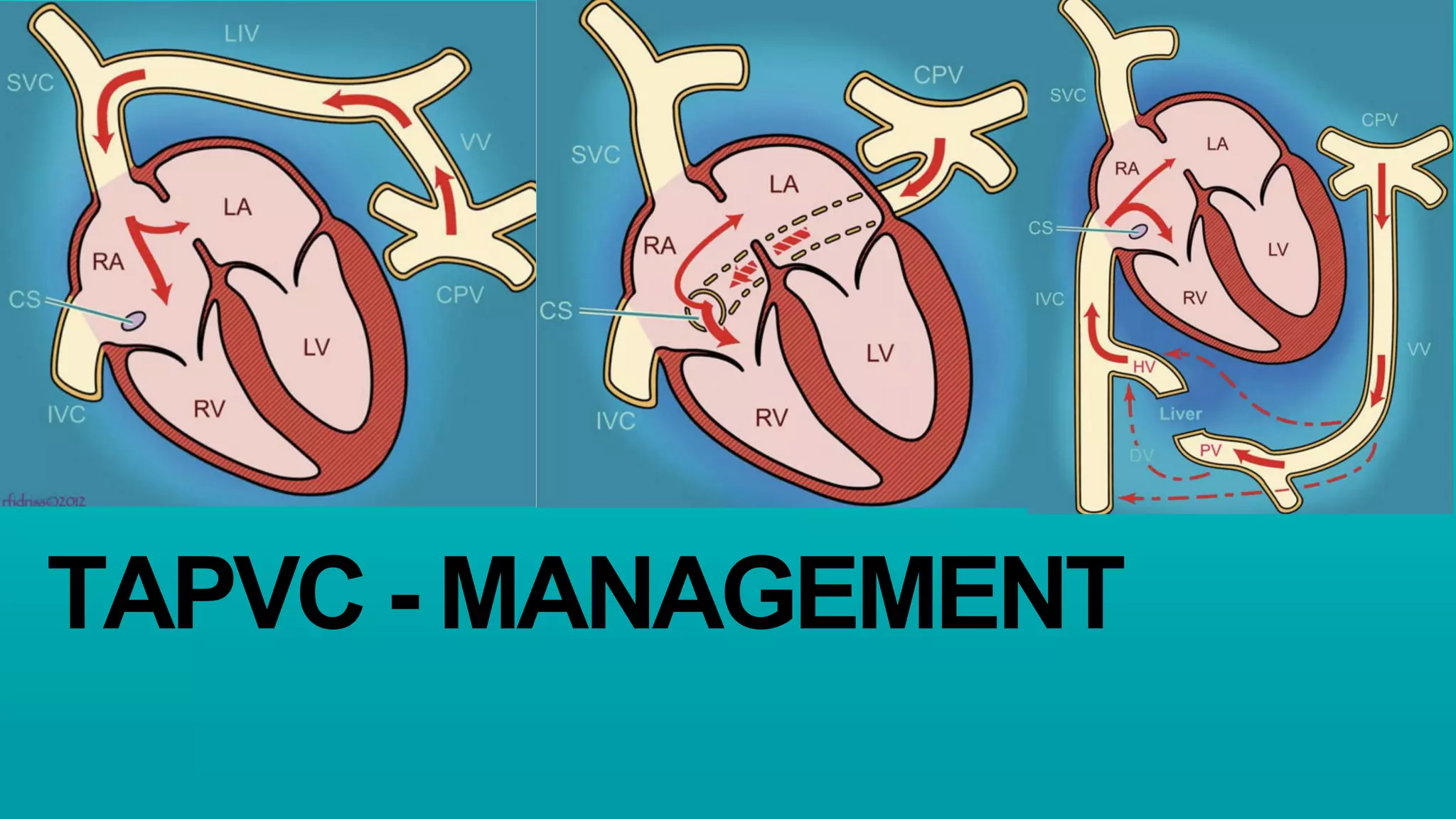
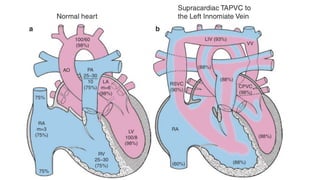
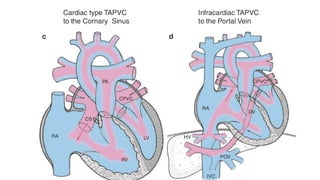
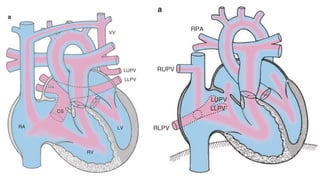
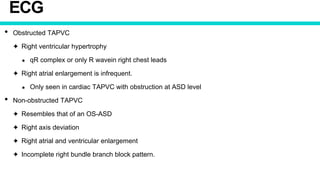
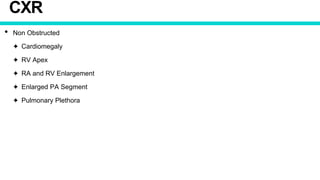
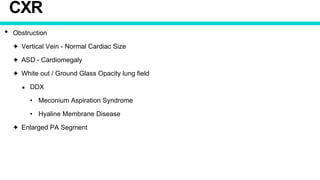
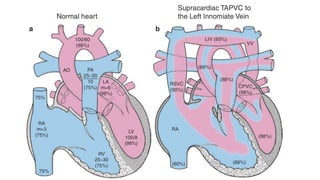
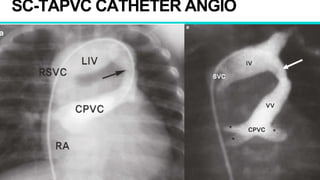
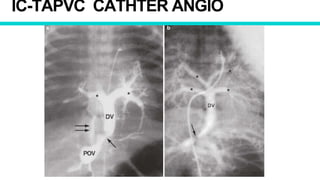
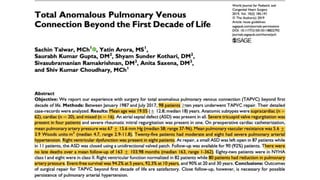
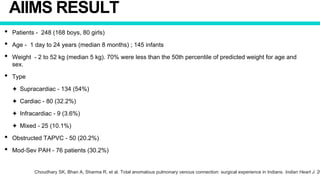
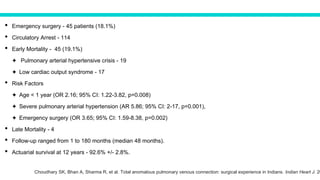
This document discusses the diagnosis and management of total anomalous pulmonary venous connection (TAPVC). It covers the types of TAPVC, diagnostic tools including ECG, CXR, echocardiography and catheterization, and surgical and interventional treatment options. The key points are:
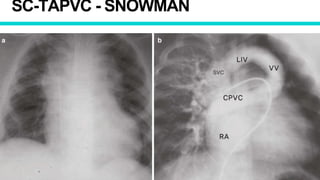
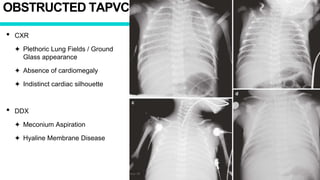
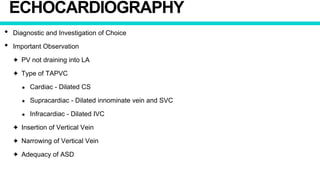
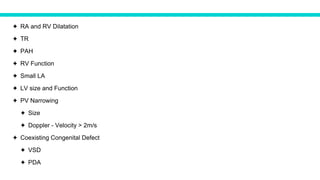
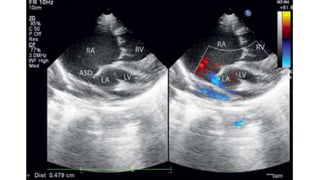
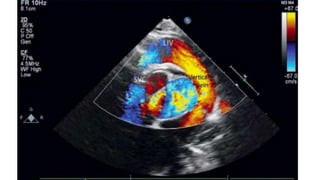
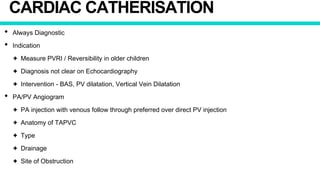
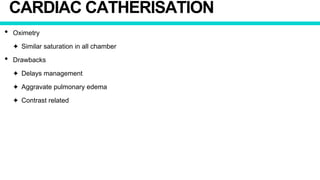
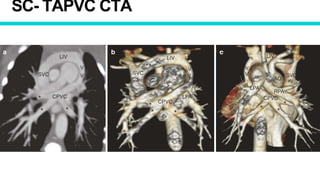
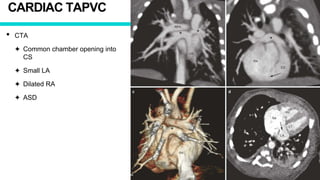
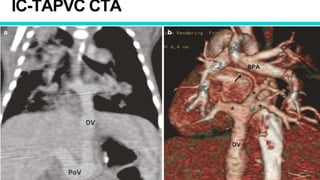
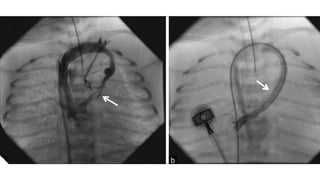
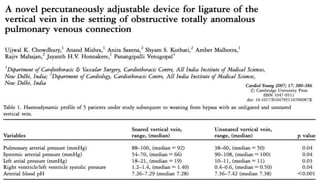
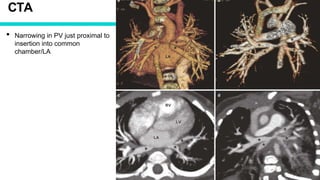
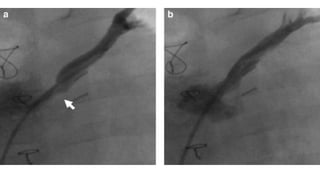
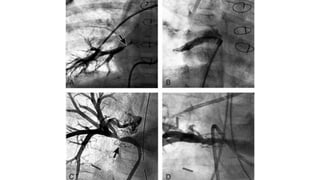
1. TAPVC is diagnosed using imaging modalities like echocardiography, CT, and catheterization to identify the anomalous pulmonary vein drainage.
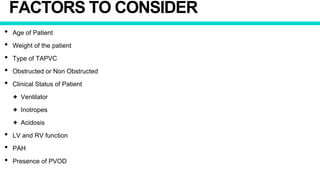
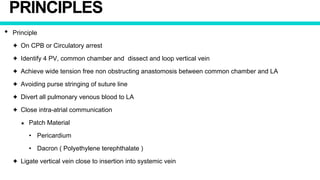
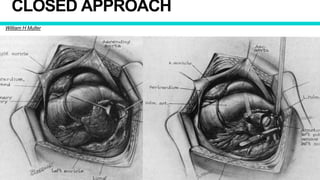
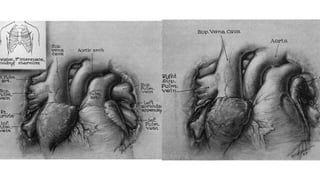
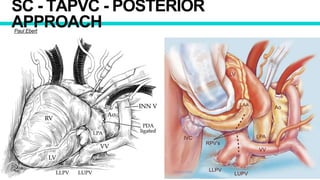
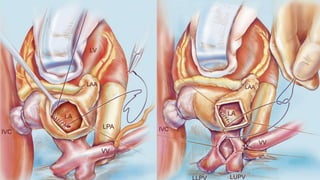
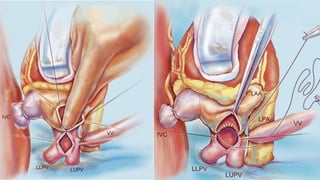
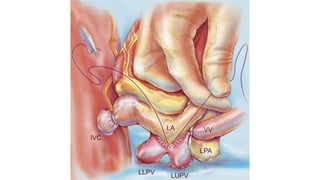
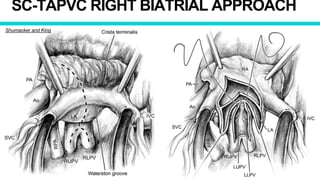
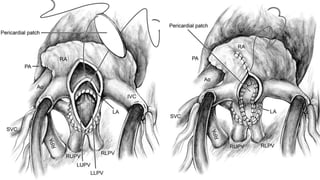
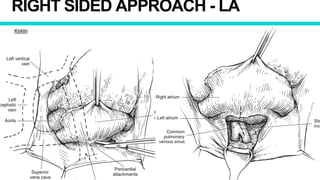
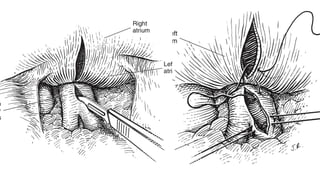
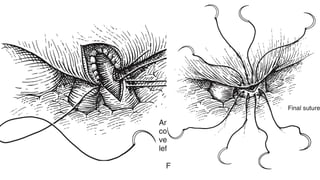
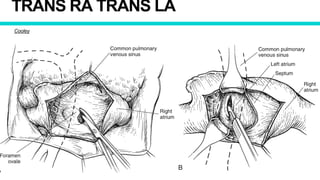
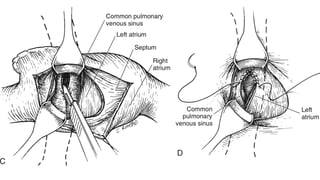
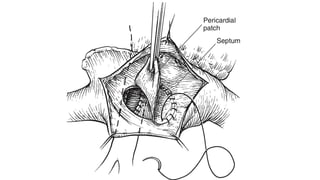
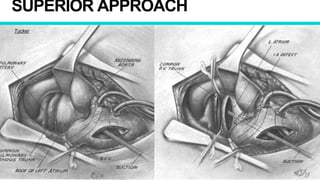
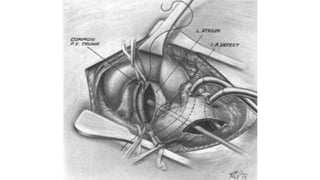
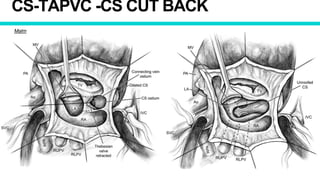
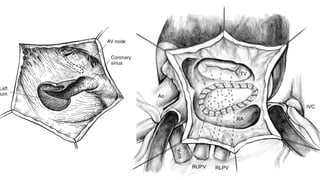
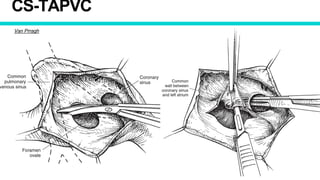
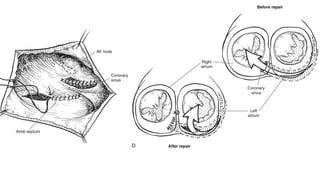
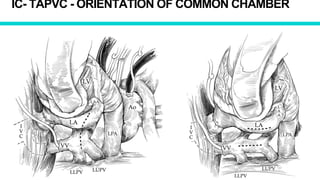
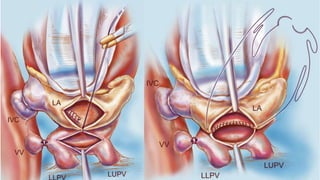
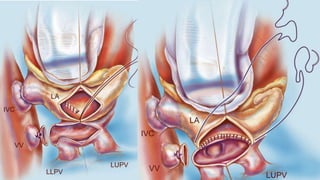
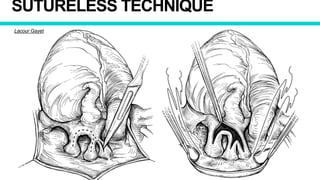
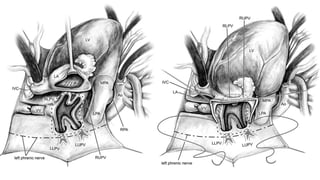
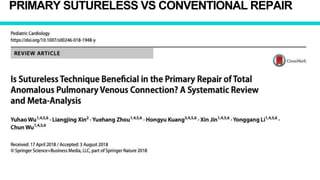
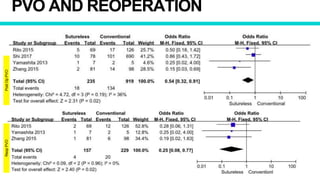
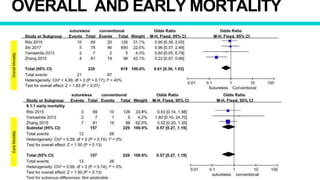
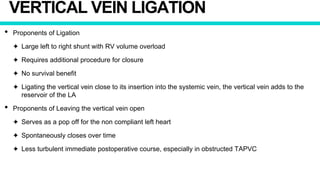
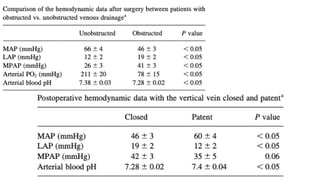
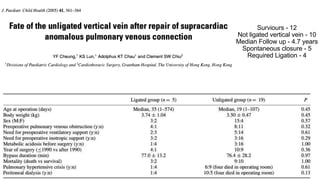
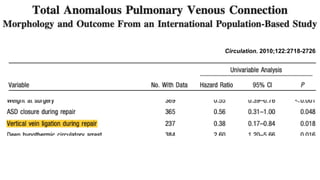
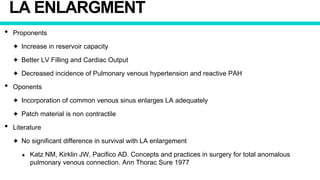
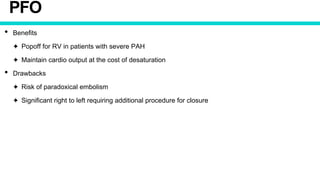
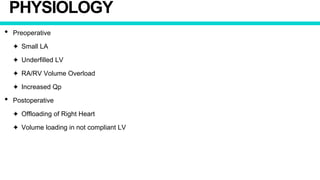
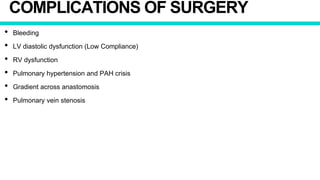
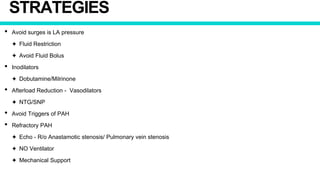
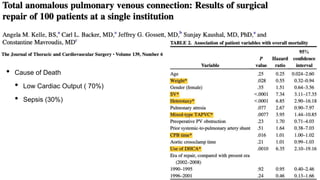
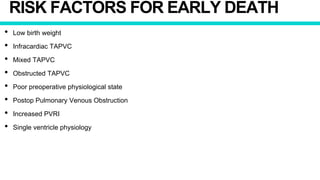
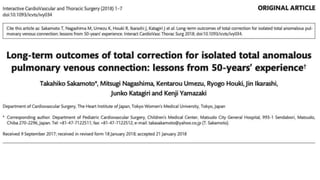
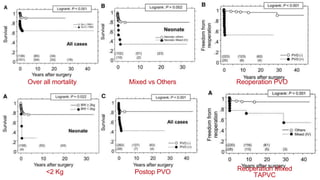
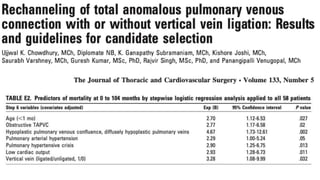
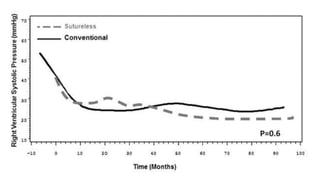
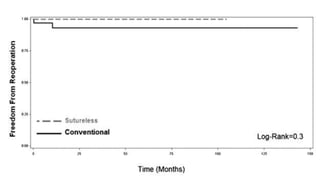
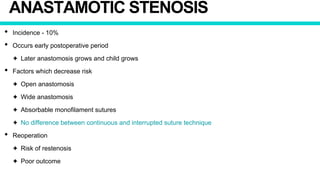
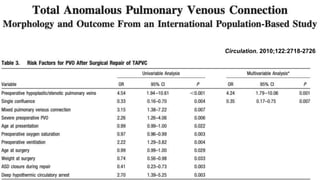
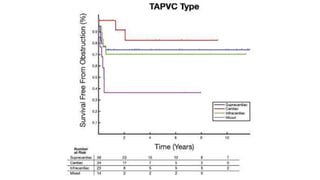
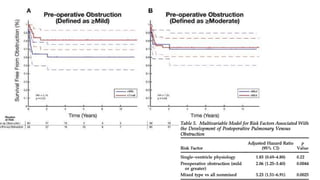
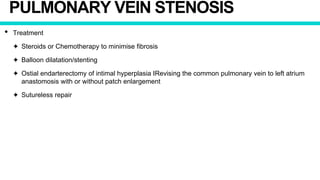
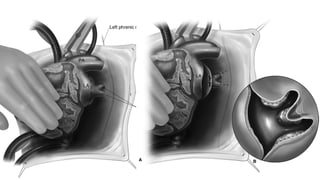
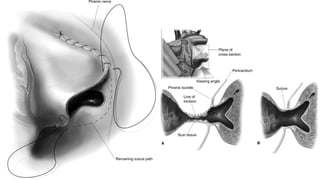
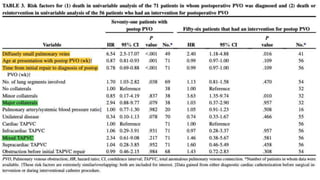
2. Surgical repair is the definitive treatment and involves anastomosis of the pulmonary veins to the left atrium. Factors like age, type of TAPVC, and presence of obstruction determine timing of surgery.
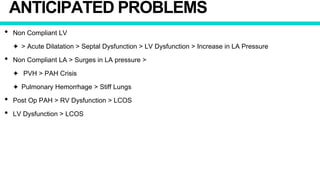
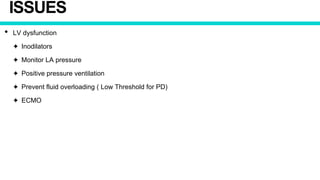
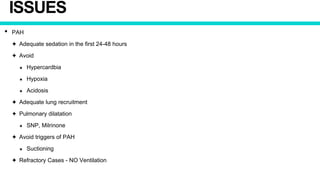
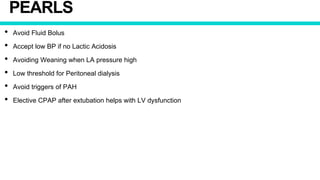
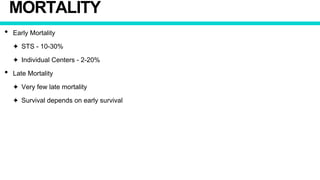
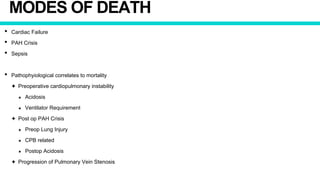
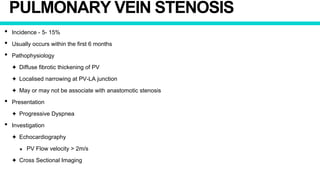
3. Post-operative management focuses on stabil