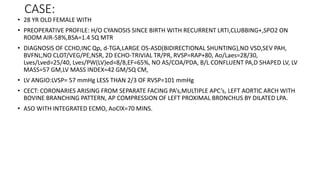
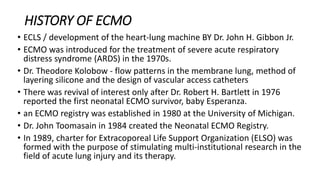
1. The document describes a case of a 28-year-old female with cyanotic congenital heart disease who underwent an arterial switch operation with integrated ECMO support.
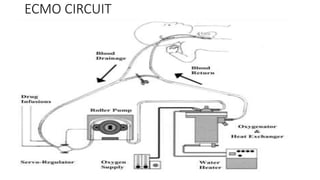
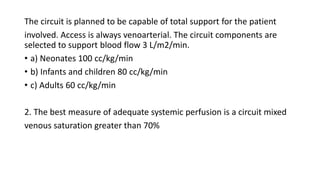
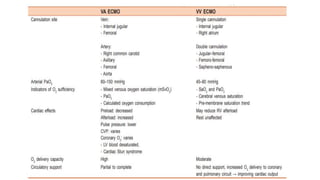
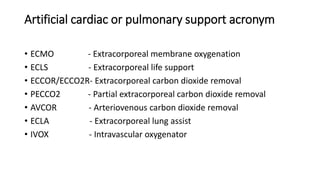
2. ECMO is a form of extracorporeal life support used for both cardiac and respiratory failure in adults. It involves pumping blood out of the body to an artificial lung for gas exchange before returning it to circulation.
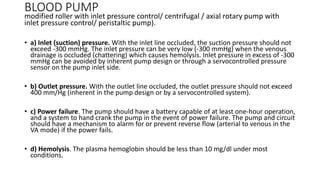
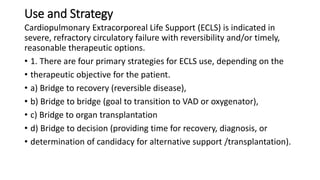
3. The key components of an ECMO circuit include a blood pump, membrane oxygenator, tubing, heat exchanger, and monitoring equipment. Proper anticoagulation and flow rates are important for safety and effectiveness.





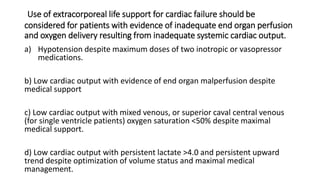
![Extracorporeal membrane oxygenation
indication indices for >80% predicted mortality
Likely to die (predicted 80% mortality)
• Oxygenation Index (OI) > 40 or > 35 for 4 hours {{OI = (MAP × FiO2 ×
100) / PaO2}}
• Ventilation Index (VI) > 90 for 4 hours {{VI = RR × PIP – PEEP/1000}}
• Alveolar–arterial oxygen difference [(A − a)DO2] >600 − 624 mmHg (at
sea level) despite 4–12 hours of medical management
(A − a)DO2 = [atmospheric pressure – 47] – (PaCO2 + PaO2)/FiO2
• PaO2 < 50 mmHg for 2–12 hours (FiO2 of 100%)
• Acute deterioration PaO2: < 30–40 mmHg (FiO2 of 100%)
• pH < 7.25 for 2 hours
• Intractable hypotension](https://image.slidesharecdn.com/adultecmo1-200916175200/85/Adult-ecmo-25-320.jpg)