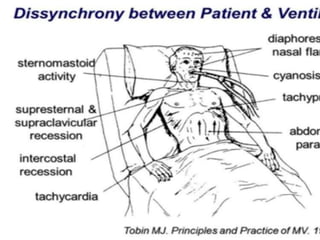
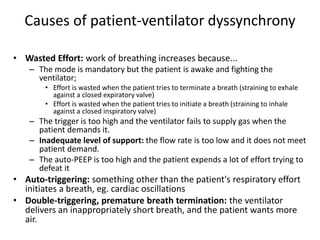
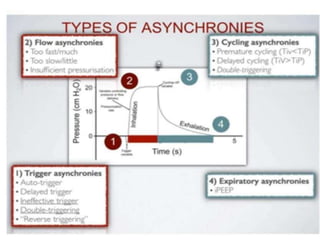
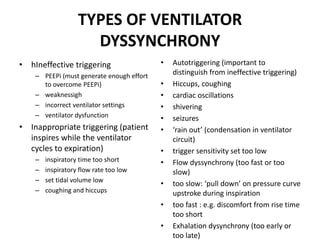
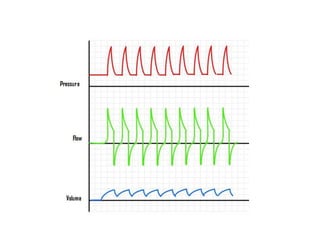
This document discusses patient-ventilator dyssynchrony, which occurs when a patient's respiratory demands are not appropriately met by the ventilator. This can increase the patient's work of breathing, lead to distress, and prolong the need for ventilation. Dyssynchrony can be caused by inappropriate ventilator settings, modes where the patient is fighting the ventilator, or issues like auto-triggering. Identifying the type and cause of dyssynchrony is important to optimize ventilator support and improve the patient experience.