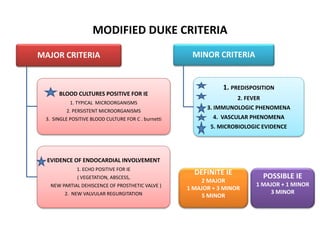
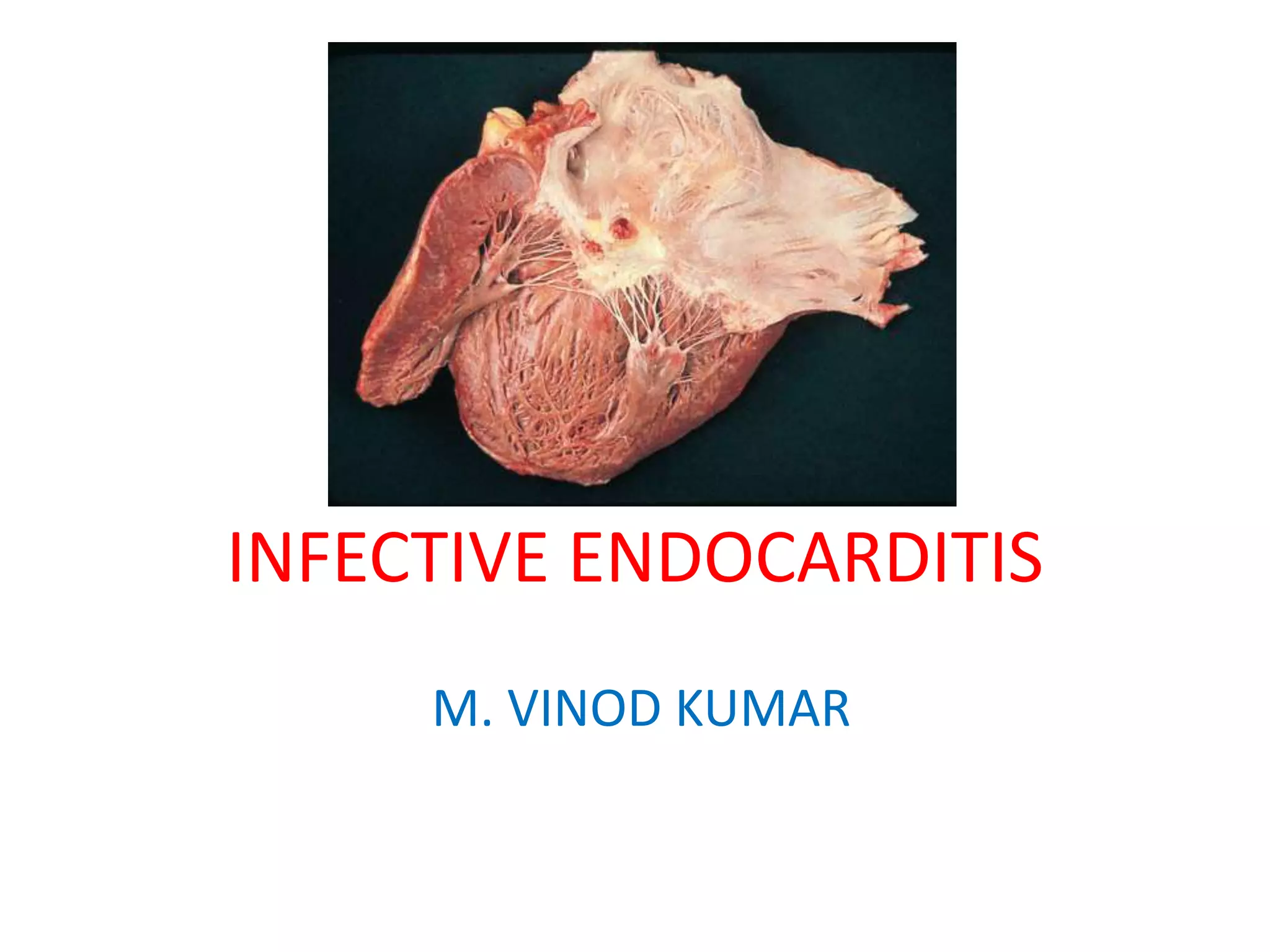
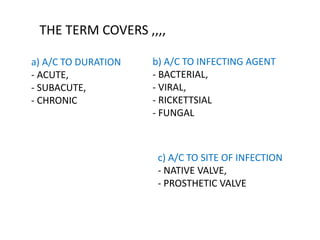
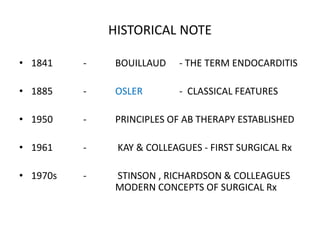
This document defines infective endocarditis and discusses its pathogenesis, clinical features, diagnosis, treatment and complications. Some key points:
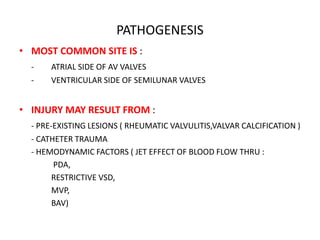
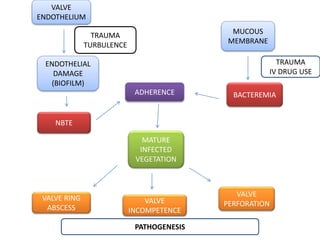
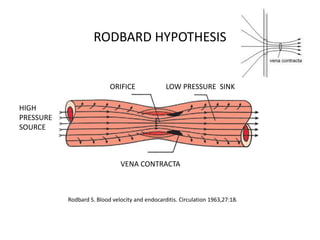
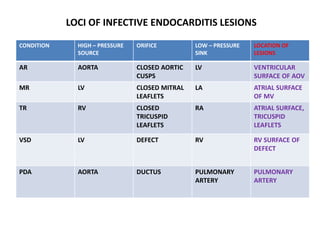
- Infective endocarditis is defined as an infection of the endocardial surface of the heart, including heart valves. It most commonly affects the atrial side of the AV valves and ventricular side of semilunar valves.
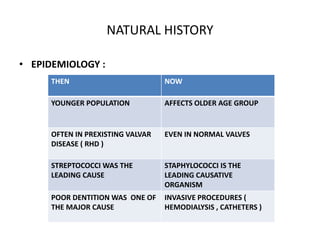
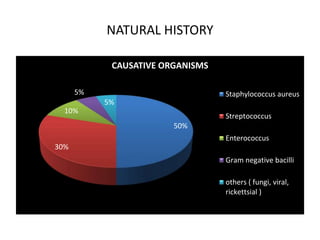
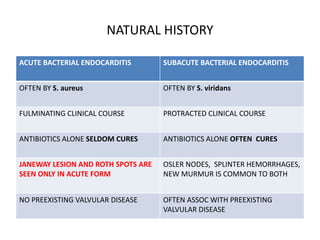
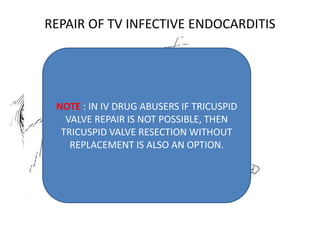
- Staphylococcus aureus is now the most common causative organism, whereas streptococci were previously more common. Risk factors include underlying heart conditions, intravenous drug use, and invasive procedures.
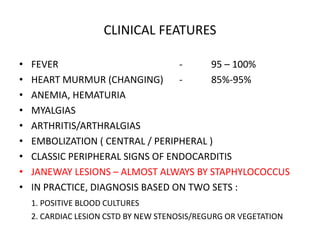
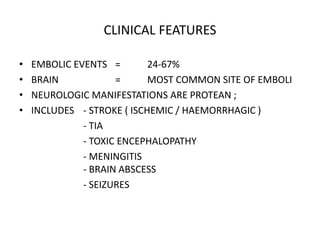
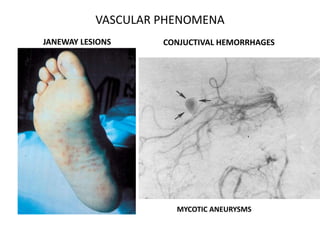
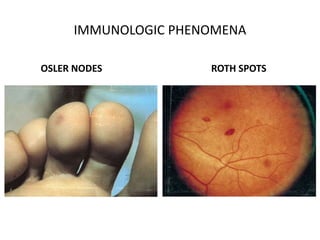
- Clinical features include fever, heart murmur, embolic events, and immunological findings like Roth spots and Osler nodes
![MORPHOLOGY
• VEGETATIONS, EROSIVE CAVITIES – VENTRICULAR ASPECT OF AOV, ATRIAL
ASPECT OF MV
• OFTEN RESULT IN DISCONTINUITY AT
THE VA OR AV JUNCTION
• DISCRETE PERFORATIONS OF AOV
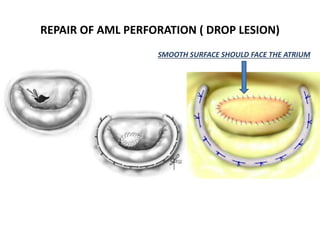
• DROP LESIONS ON AML
• PERIANNULAR PSEUODANEURYSMS
/ ABSCESS [ AOV > MV ]](https://image.slidesharecdn.com/infectiveendocardiitis-kkln-200916181934/85/Infective-endocardiitis-11-320.jpg)