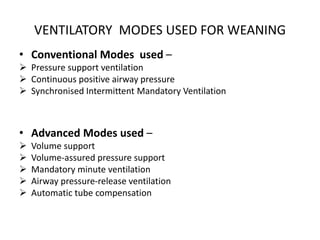
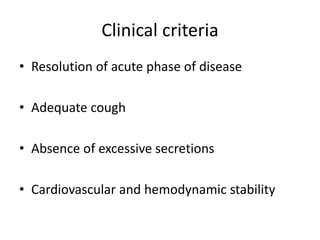
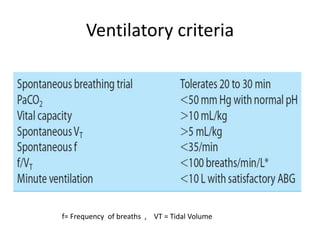
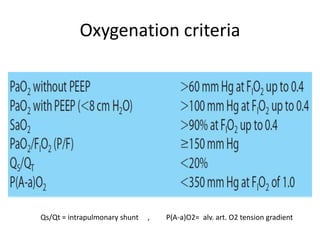
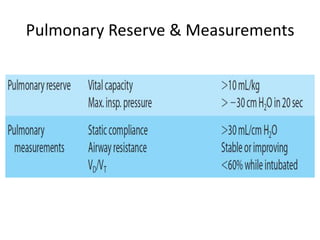
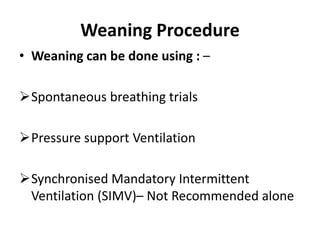
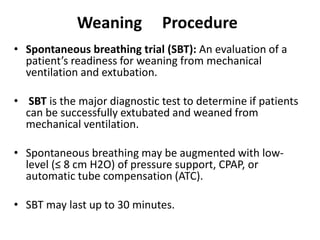
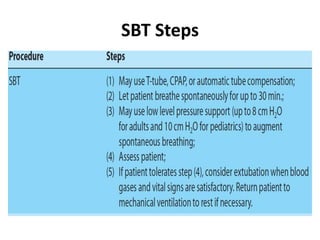
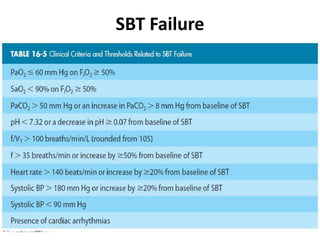
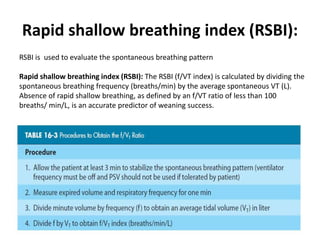
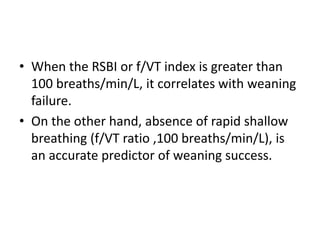
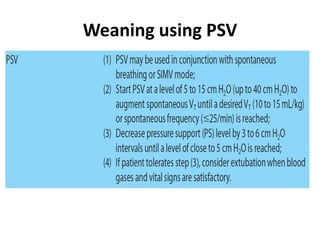
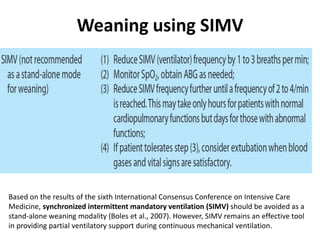
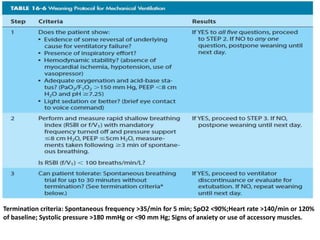
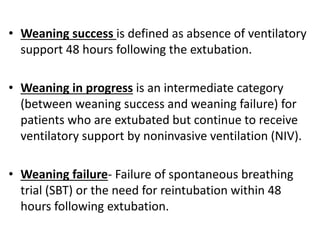
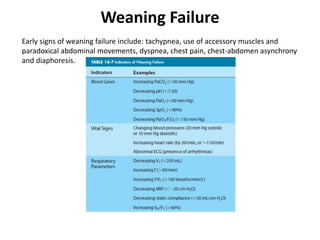
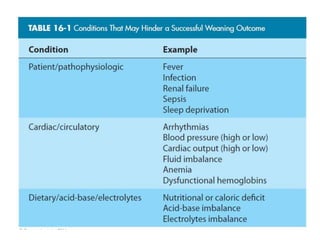
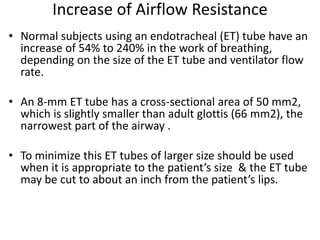
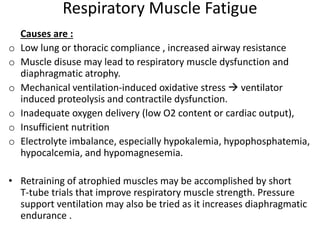
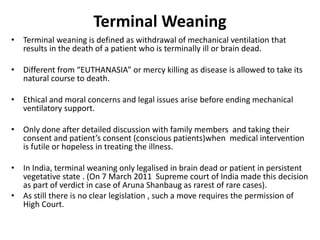
Weaning from mechanical ventilation is a critical process involving the gradual withdrawal of mechanical support as patients regain spontaneous breathing capability after recovering from their acute condition. Successful weaning necessitates careful evaluation of clinical, ventilatory, and oxygenation criteria, with various modes and trials employed to assess readiness for extubation. Challenges such as weaning failure can arise due to respiratory muscle fatigue or increased airflow resistance, and ethical considerations are pivotal in cases of terminal weaning.