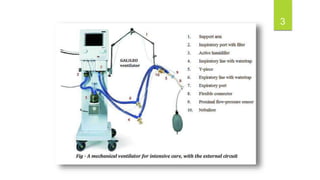
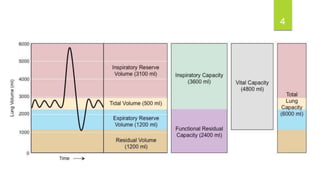
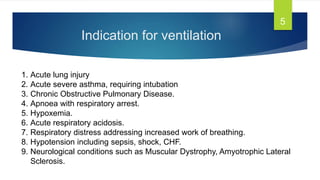
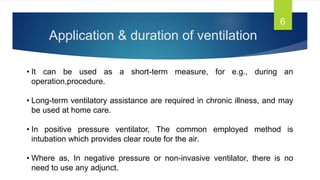
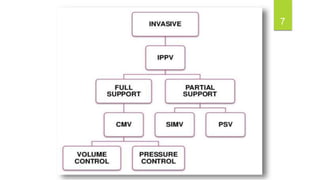
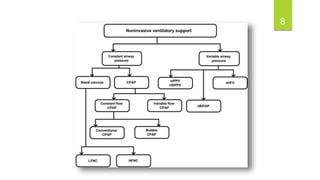
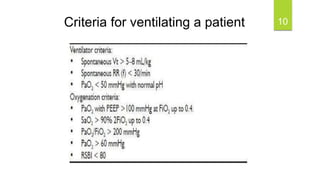
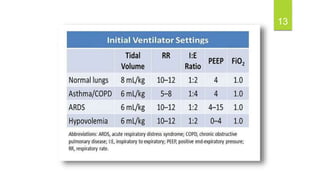
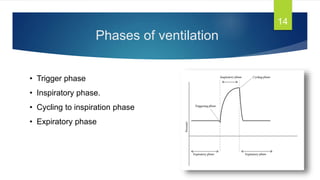
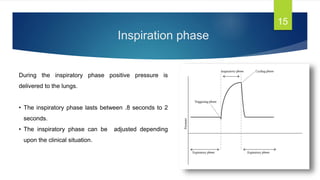
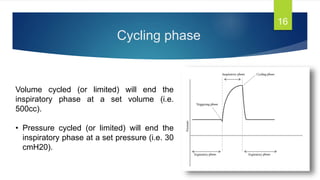
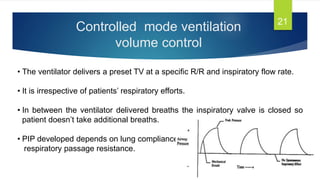
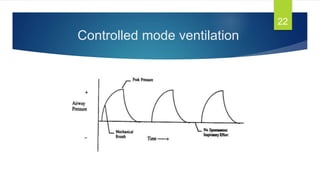
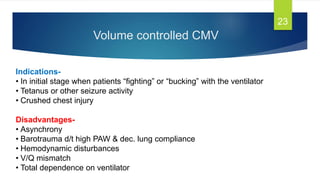
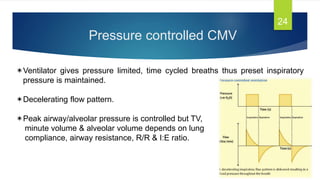
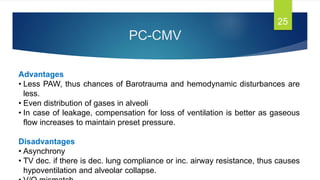
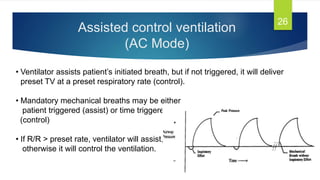
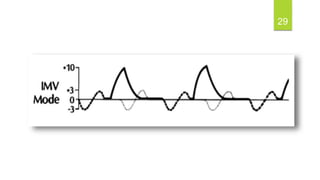
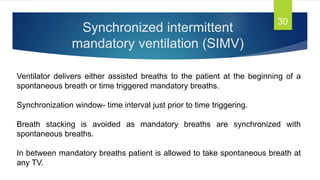
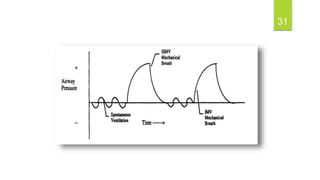
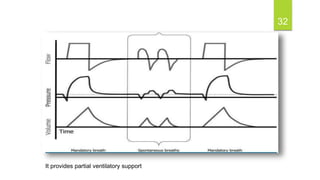
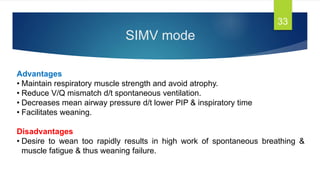
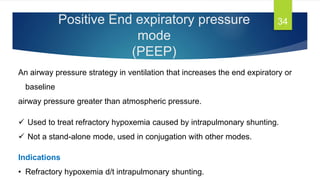
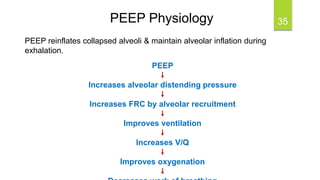
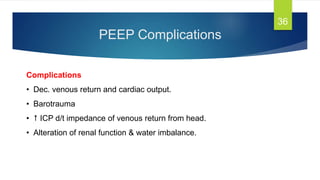
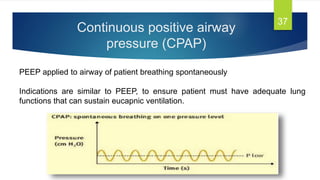
The document provides detailed insights into mechanical ventilators, including their indications, modes, and settings for proper patient ventilation. It outlines criteria for patient ventilation, the phases of ventilation, and various modes like volume control, pressure control, and assisted control, highlighting advantages and disadvantages of each. Additionally, it discusses specialized techniques like PEEP and CPAP, along with guidelines for weaning patients off mechanical support.