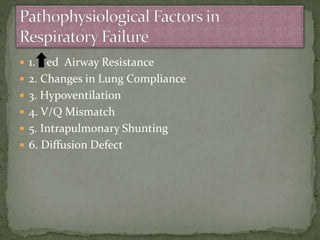
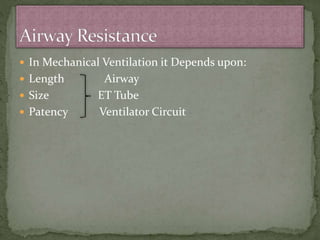
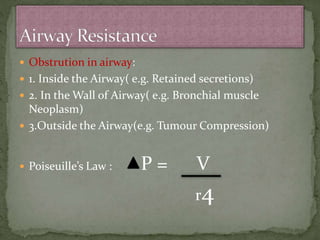
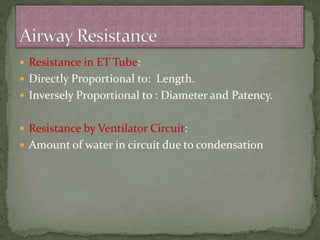
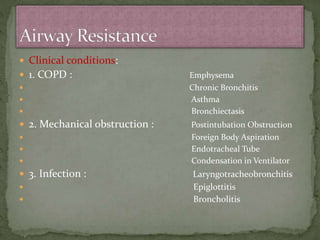
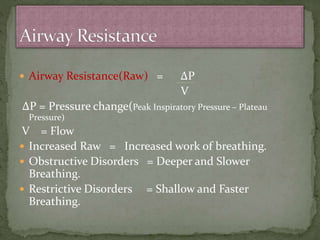
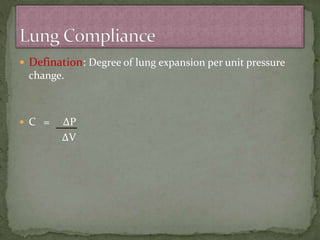
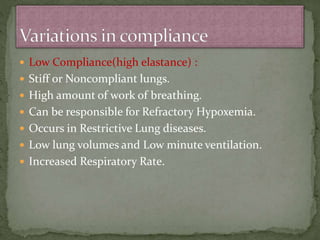
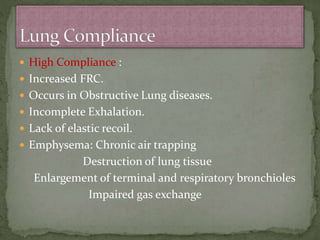
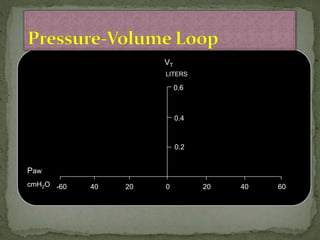
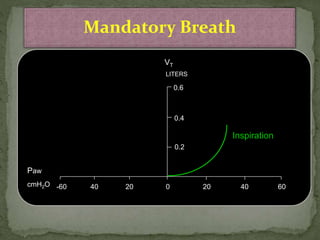
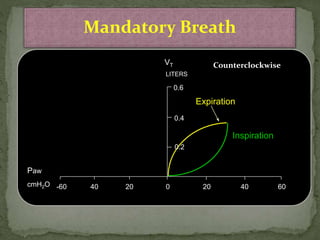
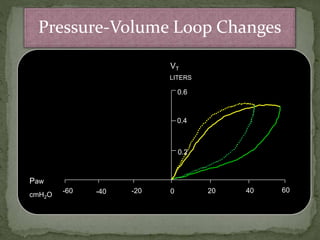
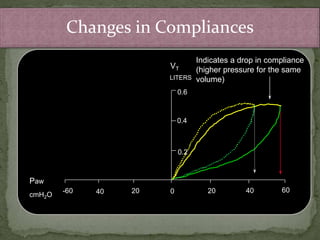
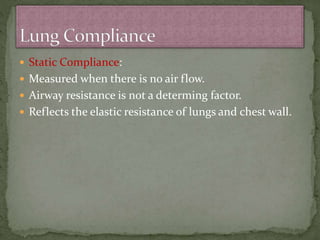
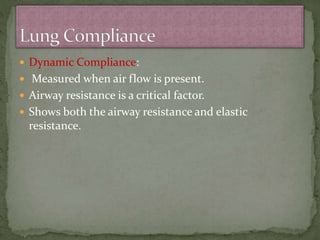
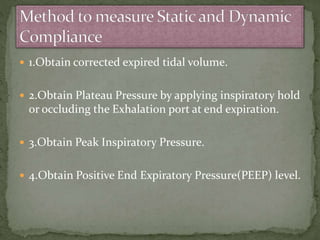
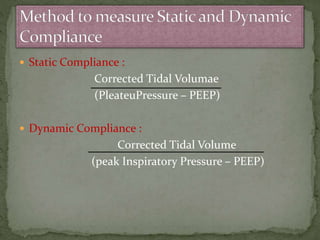
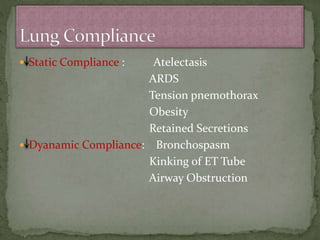
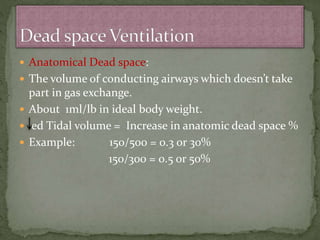
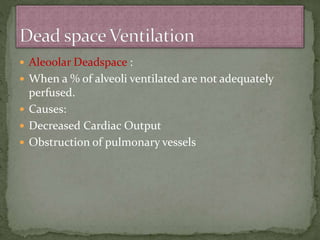
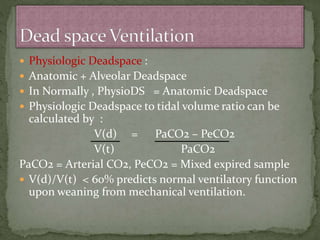
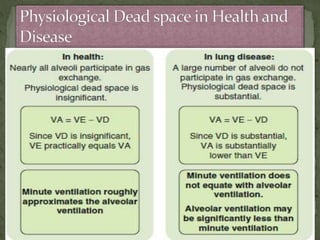
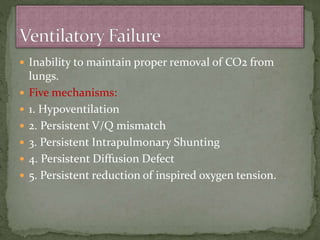
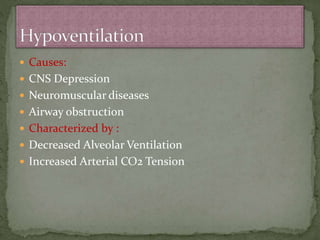
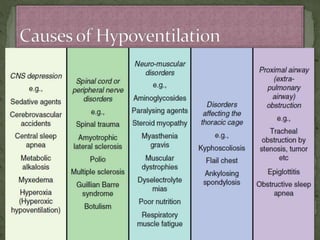
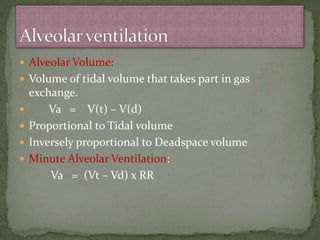
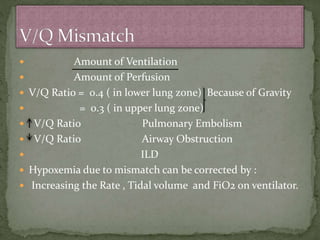
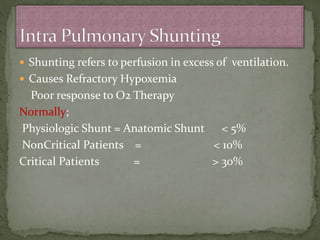
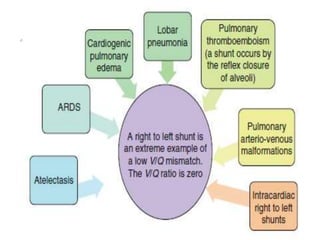
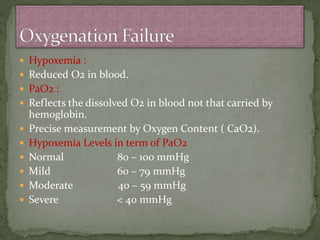
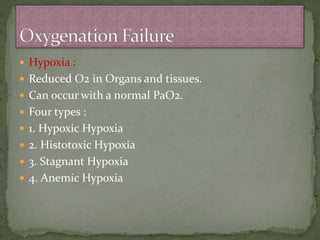
The document discusses mechanical ventilation and factors that influence airway resistance. It notes that patients may require mechanical ventilation due to ventilatory or oxygenation failure. Several factors can affect airway resistance, including changes in lung compliance, airway obstructions, and infections. The length and diameter of the endotracheal tube and patency of the ventilator circuit also impact resistance. Clinical conditions like COPD, asthma, and infections can further increase resistance. Proper assessment of compliance, dead space, and causes of hypoxemia are important for effective mechanical ventilation.