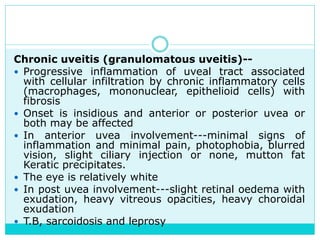
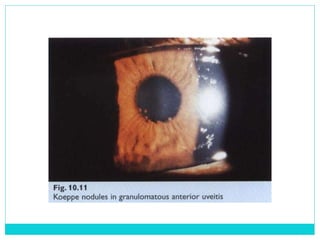
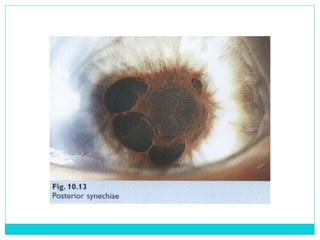
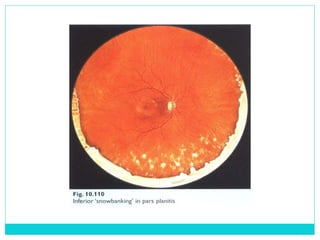
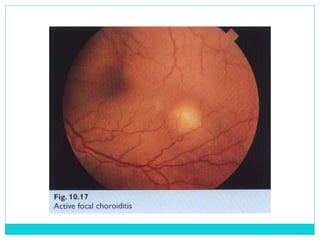
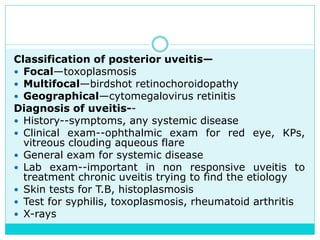
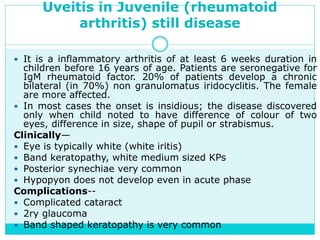
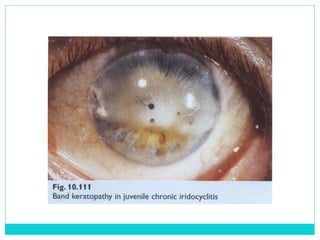
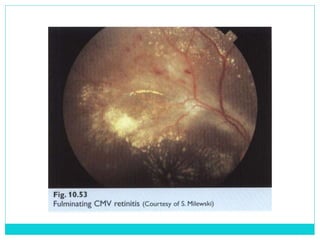
The document provides information on the uveal tract, which consists of the iris, ciliary body, and choroid. It describes the anatomy, histology, and functions of each part of the uvea. Signs and symptoms of uveal inflammation/uveitis are discussed, including anterior uveitis characterized by pain, photophobia, cells and flare in the anterior chamber, and keratic precipitates. Chronic/granulomatous uveitis can cause nodules on the iris and chronic inflammation. Posterior uveitis may involve the choroid and retina without anterior chamber signs.