The document provides details on the anatomy, histology, functions, blood supply, innervation, and common diseases of the cornea. It can be summarized as follows:
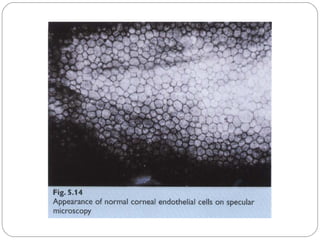
1) The cornea is the transparent front part of the eye that allows light to enter. It has five layers - epithelium, Bowman's layer, stroma, Descemet's membrane, and endothelium.
2) The cornea receives nutrients through diffusion from surrounding blood vessels and tears. Its transparency is maintained by its avascular nature and orderly arrangement of collagen fibers.
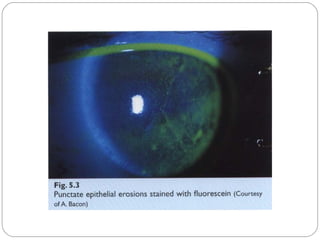
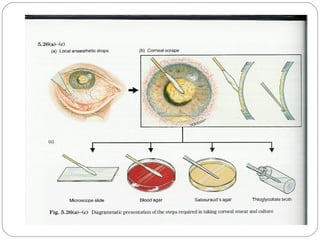
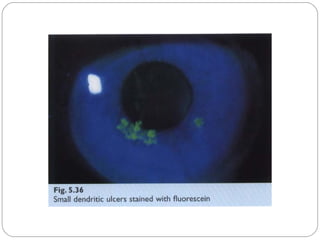
3) Common corneal diseases include infections like bacterial, fungal, and viral keratitis. Bacterial keratitis is usually caused by staphyloc












































































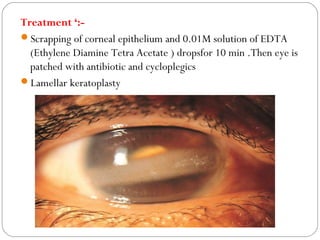
![Keratomalacia (Nutritional
keratitis )--
Softening of the cornea .Occur in children due to vit A
deficiency .Conjunctiva is dry [xerosis conjunctiva]
(Xeropthalmia) with Bitot Spots .Cornea is soft and insensitive
and no or minimal inflammatory reaction
Treatment :- general treatment by fluids , plasma proteins , vit A
drops .Local treatment and treatment or ulcer and vit A
ointment](https://image.slidesharecdn.com/cornea-171111135144/85/Cornea-88-320.jpg)