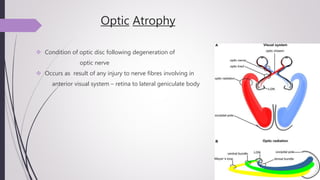
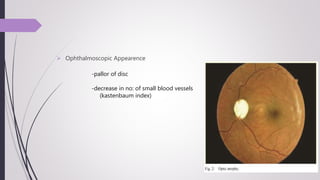
Optic atrophy is the degeneration of the optic nerve fibers leading to pallor of the optic disc. It can be classified as primary, secondary, consecutive, glaucomatous, or ischemic based on the underlying cause and appearance of the optic disc. Primary optic atrophy results from diseases proximal to the disc with a chalky white appearance. Secondary optic atrophy occurs after inflammation of the optic disc with a dirty white, blurred disc. Consecutive optic atrophy follows retinal lesions and shows a yellow waxy disc. Treatment focuses on the underlying cause when possible, but once complete atrophy occurs, vision cannot be recovered.