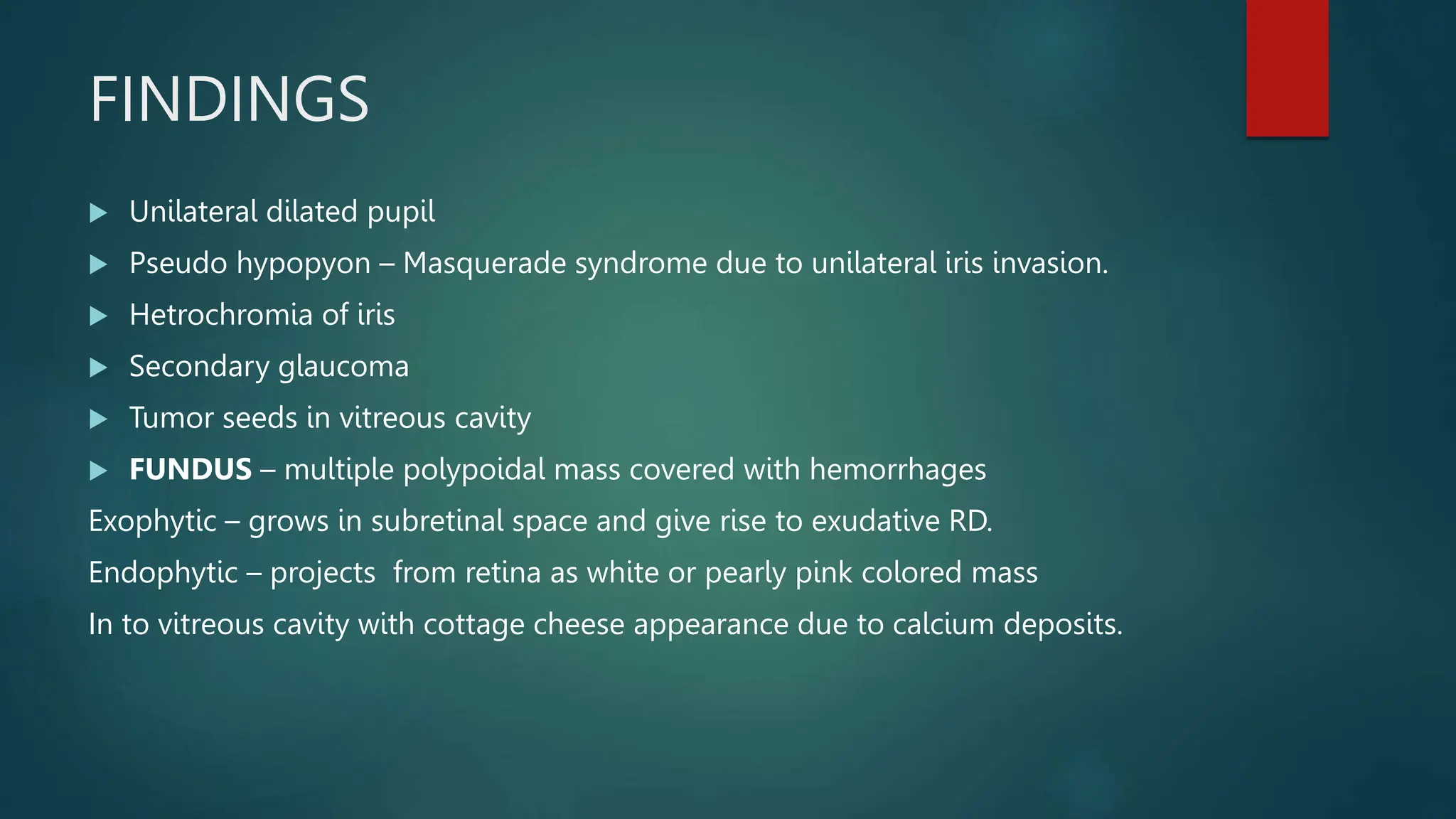
This document summarizes various retinal conditions including retinal detachment, retinoblastoma, and retinitis pigmentosa. It describes the classification, causes, clinical features, investigations, and treatments of these conditions. Retinal detachment can be rhegmatogenous, tractional, or exudative in nature. Retinoblastoma is a malignant tumor of childhood that may appear as a white pupil reflex and is typically treated with chemotherapy, radiation, or enucleation. Retinitis pigmentosa is a genetic retinal dystrophy characterized by night blindness and bony spicule pigmentation.