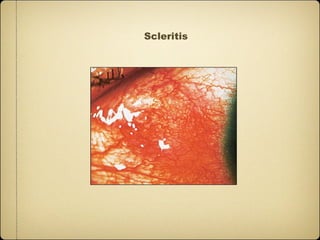
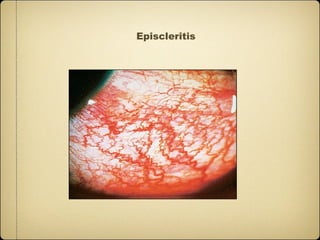
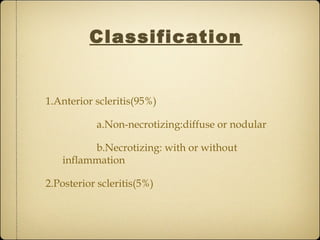
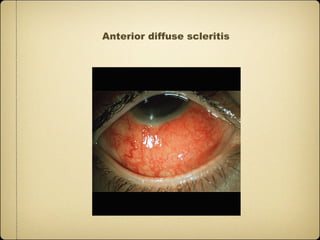
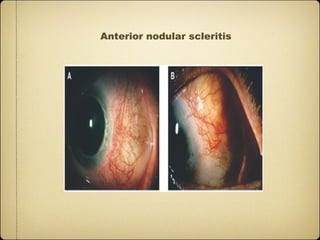
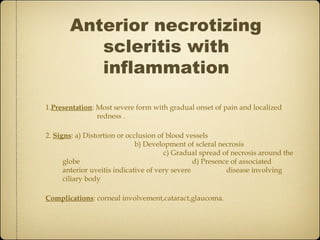
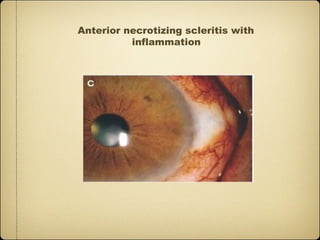
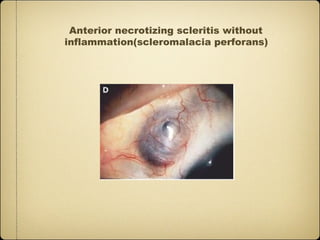
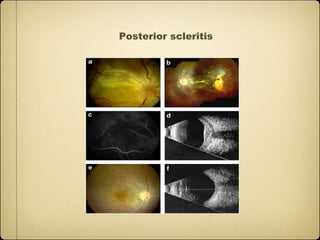
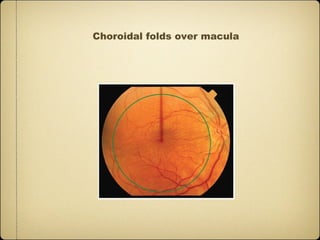
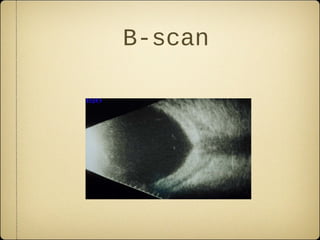
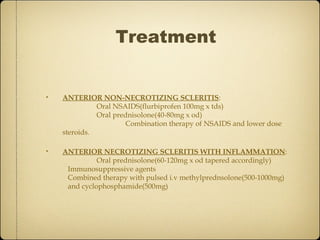
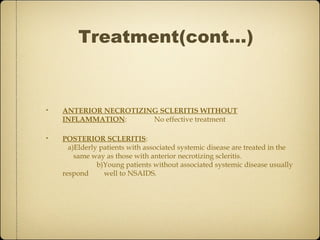
This document discusses scleritis, an inflammation of the sclera. It defines scleritis and notes it is less common than episcleritis. Scleritis can be classified as anterior or posterior, with anterior scleritis subdivided into non-necrotizing diffuse/nodular or necrotizing forms with or without inflammation. Associated systemic diseases are common in 45% of patients. Signs, symptoms, investigations, and treatment are described depending on the classification of scleritis. Surgical treatment may be needed for extreme scleral thinning or corneal complications.