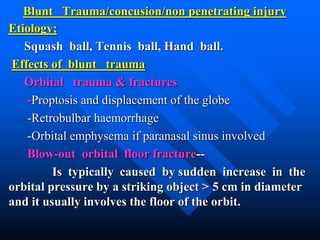
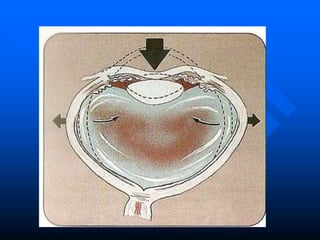
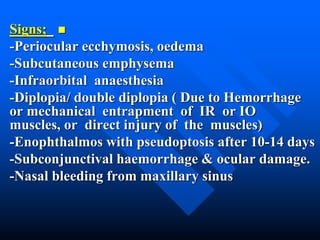
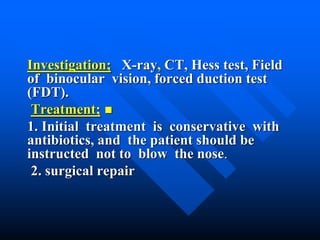
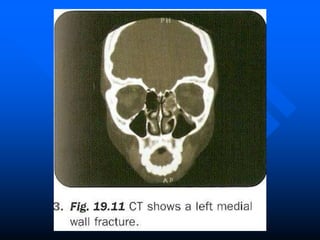
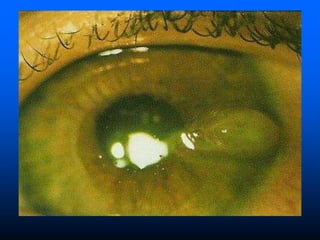
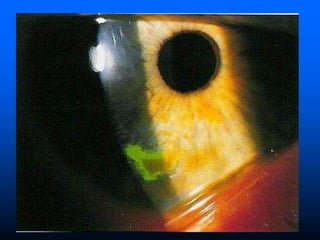
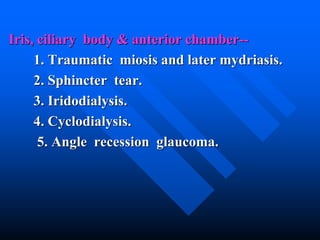
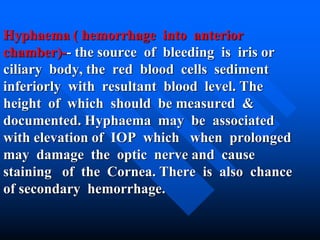
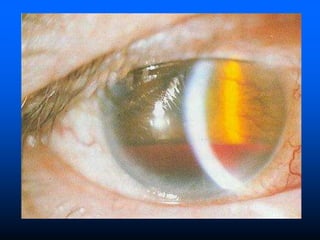
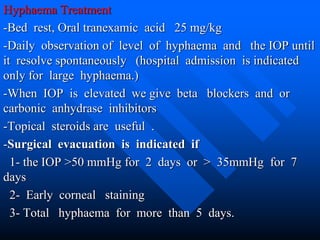
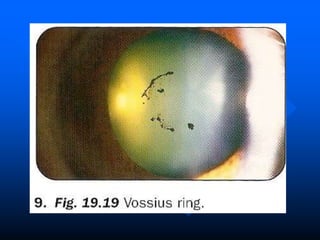
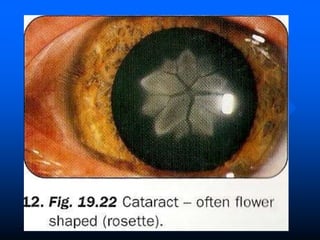
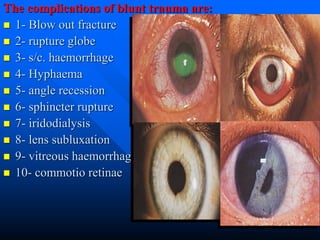
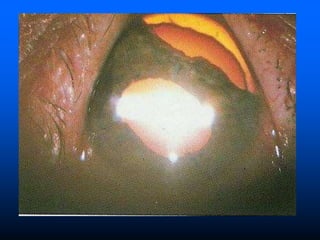
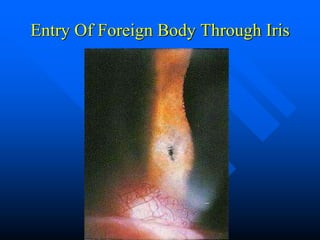
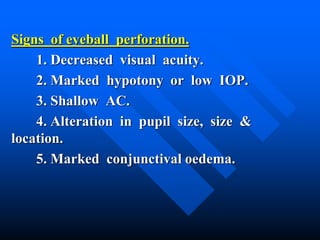
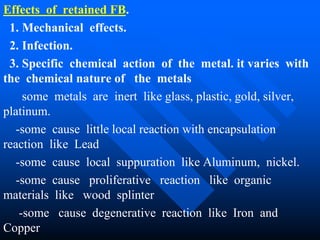
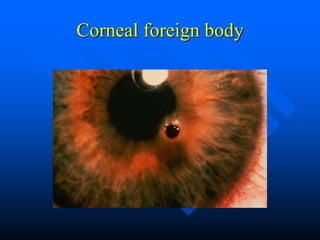
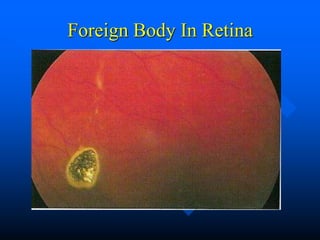
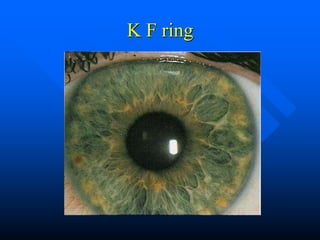
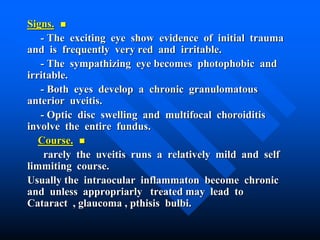
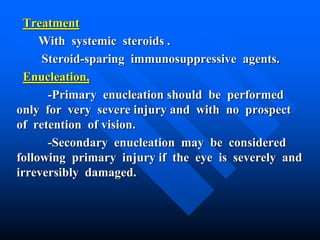
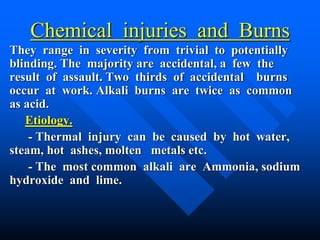
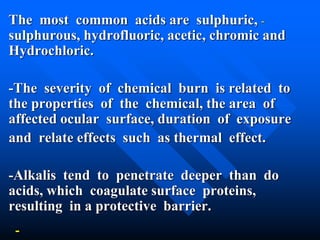
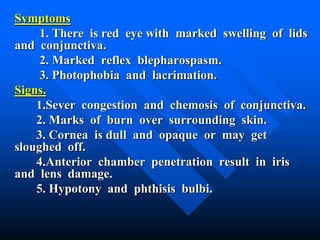
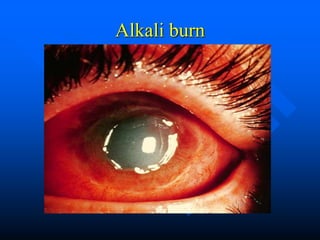
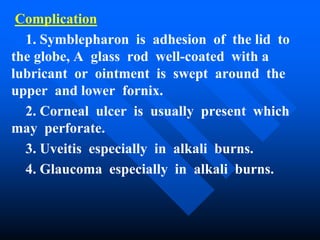
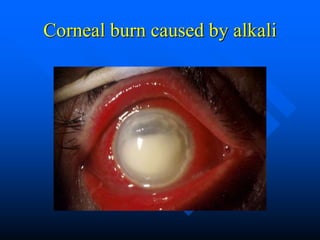
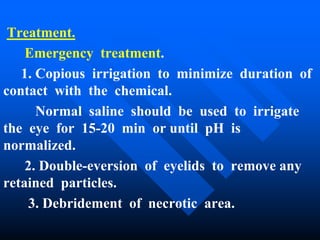
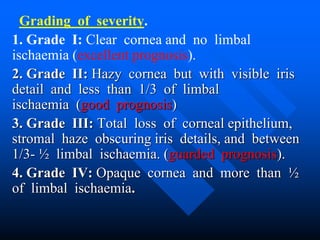
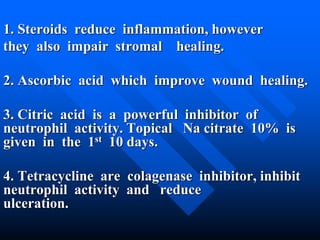
This document summarizes ocular trauma including extraocular foreign bodies, blunt trauma, penetrating trauma, and chemical injuries. It describes signs, symptoms, complications, investigations, and treatments for various types of eye injuries including hyphema, blowout fractures, iris tears, retinal detachment, and intraocular foreign bodies. Surgical management aims to repair wounds, remove foreign bodies or infected tissue, and prevent infections like endophthalmitis or sympathetic ophthalmia which can spread between eyes. Prognosis depends on severity and timing of treatment for the initial trauma.