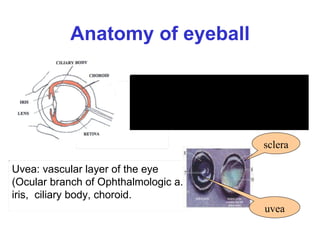
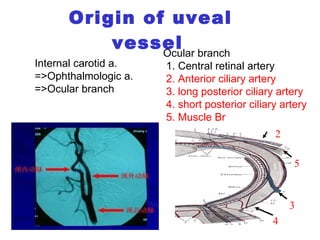
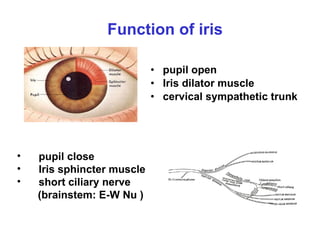
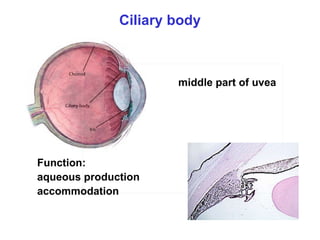
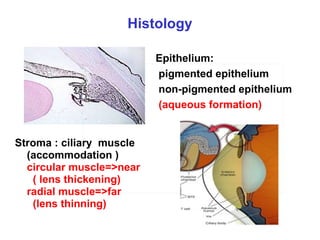
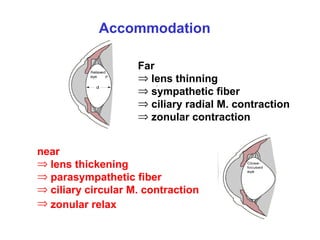
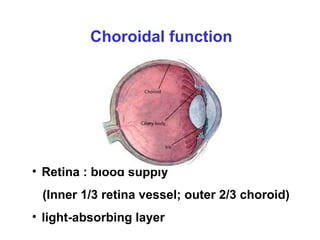
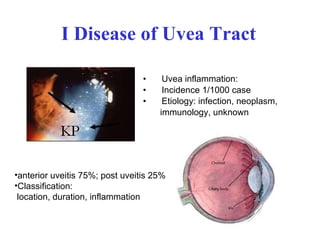
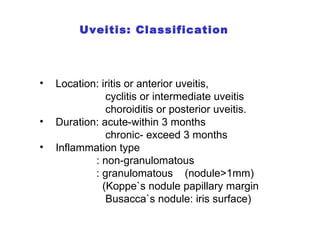
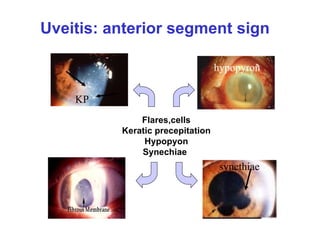
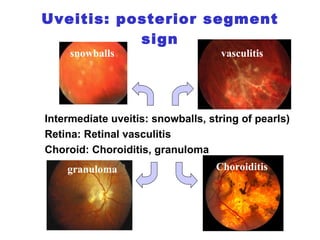
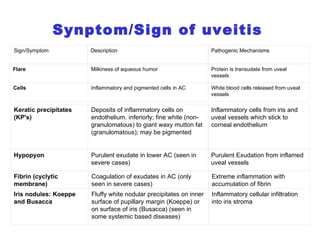
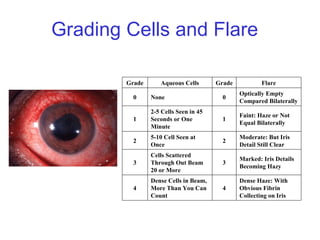
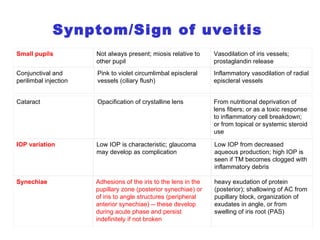
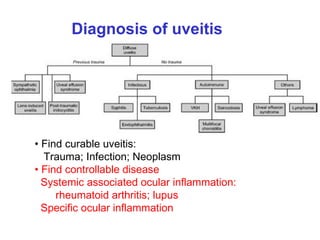
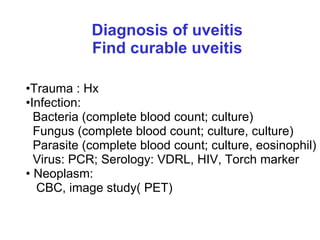
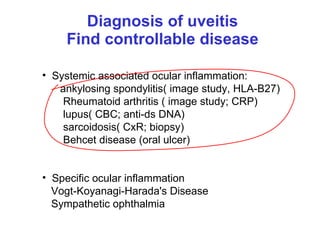
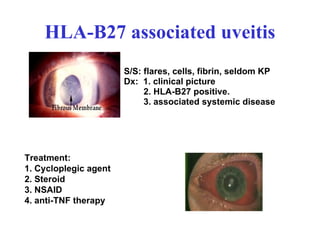
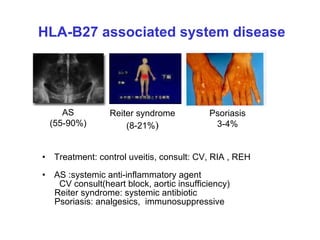
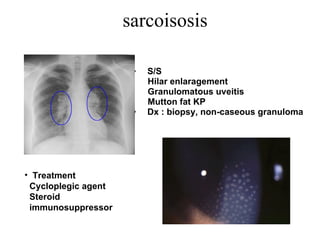
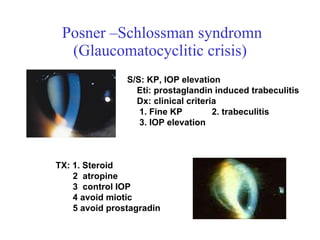
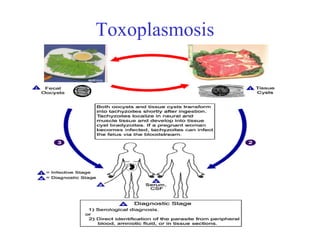
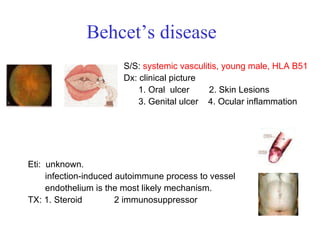
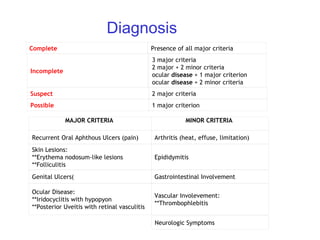
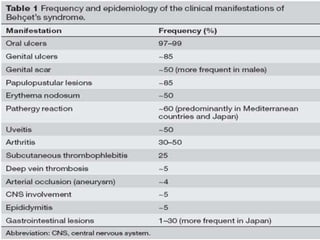
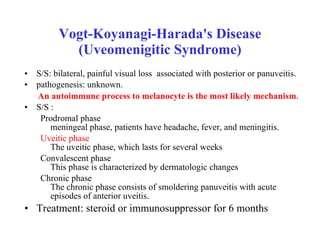
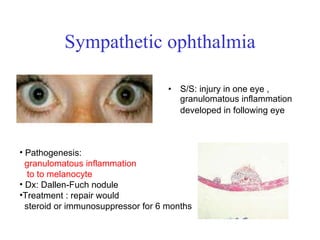
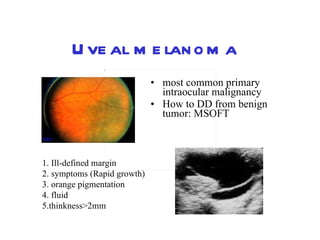
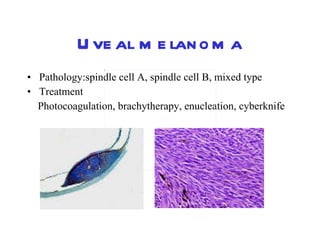
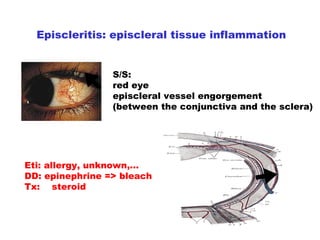
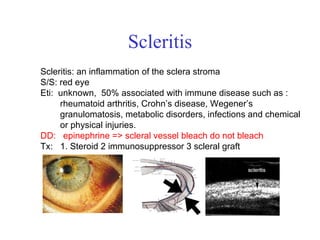
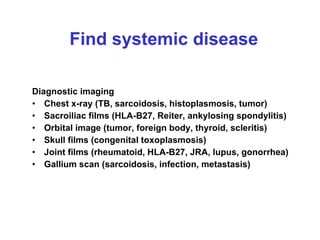
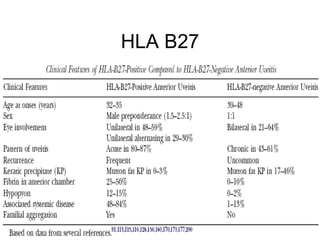
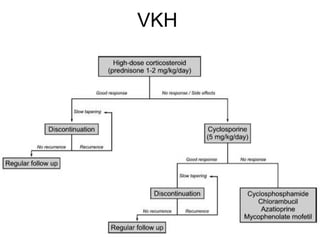
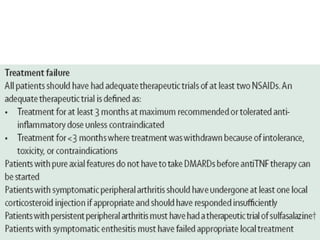
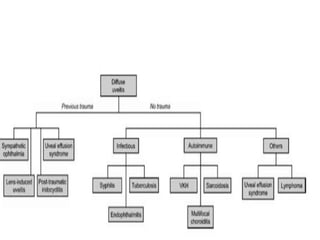
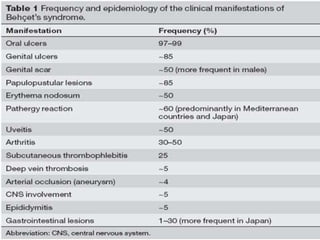
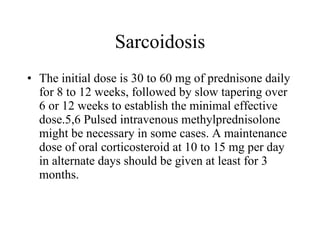
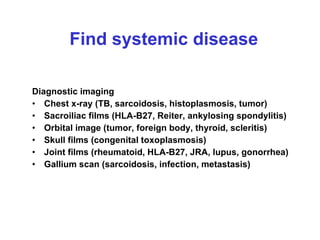
The document discusses anatomy and diseases of the eye. It describes the layers of the eyeball including the uvea and sclera. Various types of uveitis are classified and their symptoms, signs, etiologies, and treatments are explained. Specific uveitic entities like HLA-B27 associated uveitis, sarcoidosis, and toxoplasmosis are also summarized along with their diagnostic approach and management. Uveal tumors and scleral diseases are briefly covered as well.