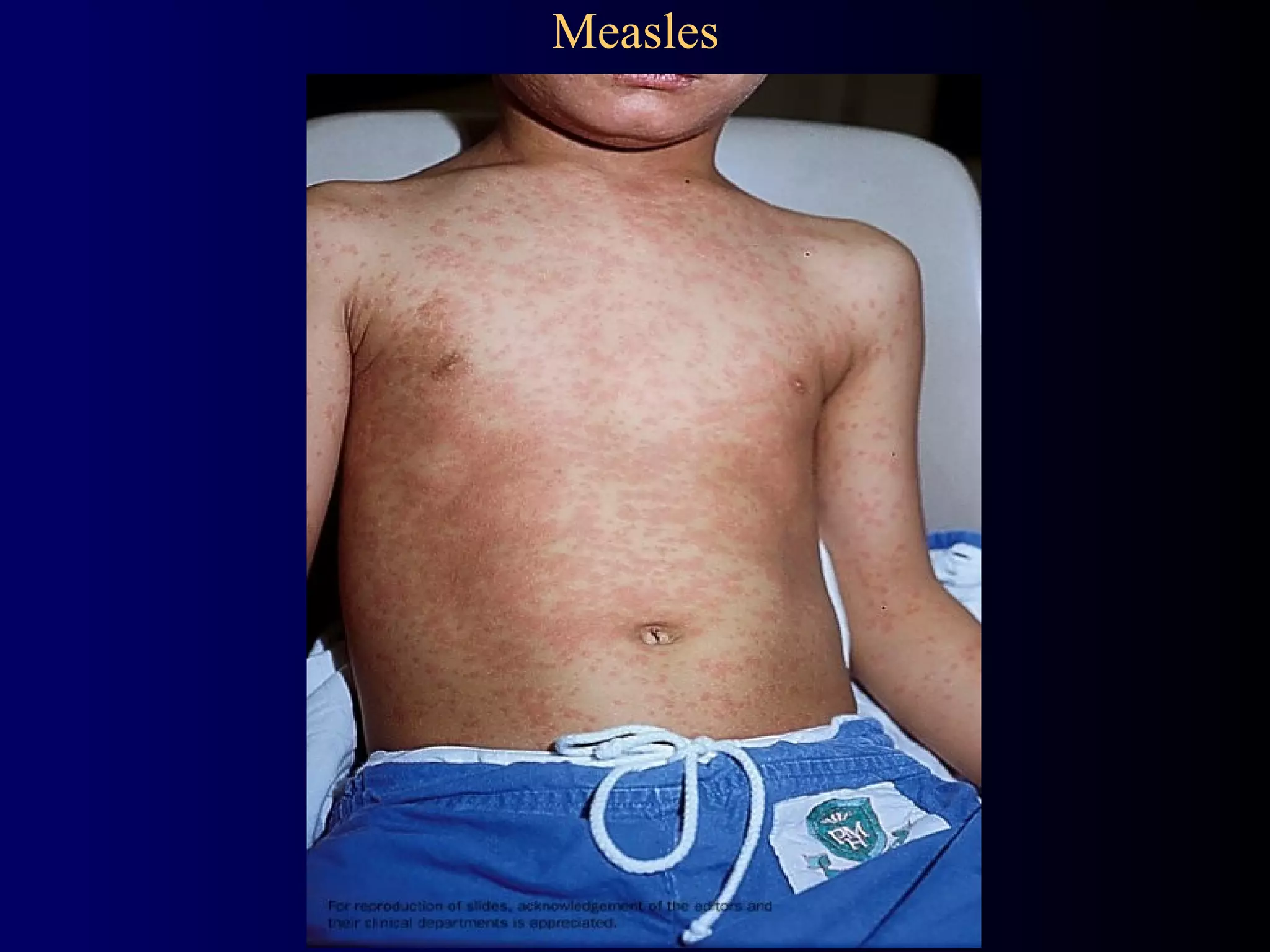
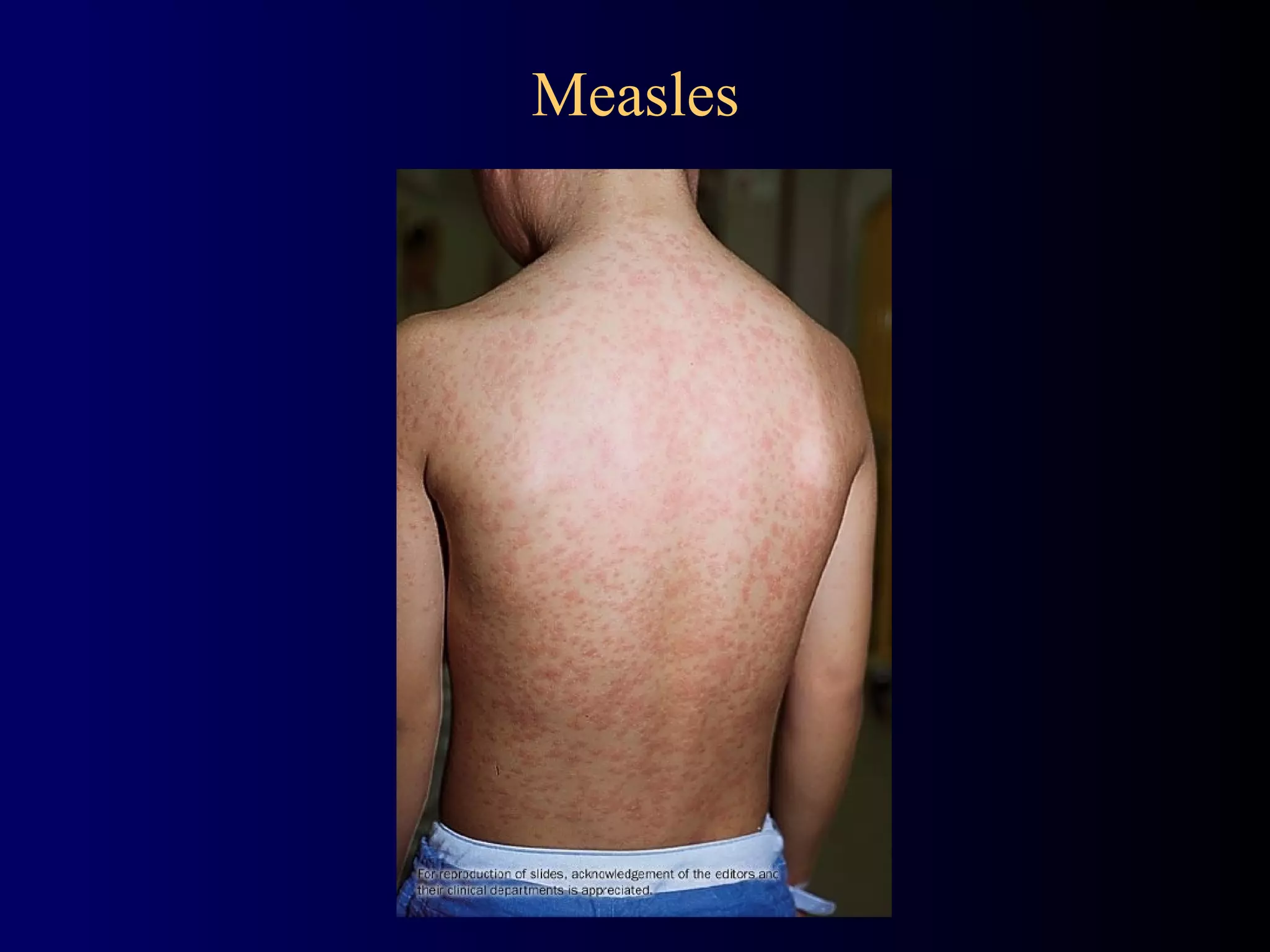
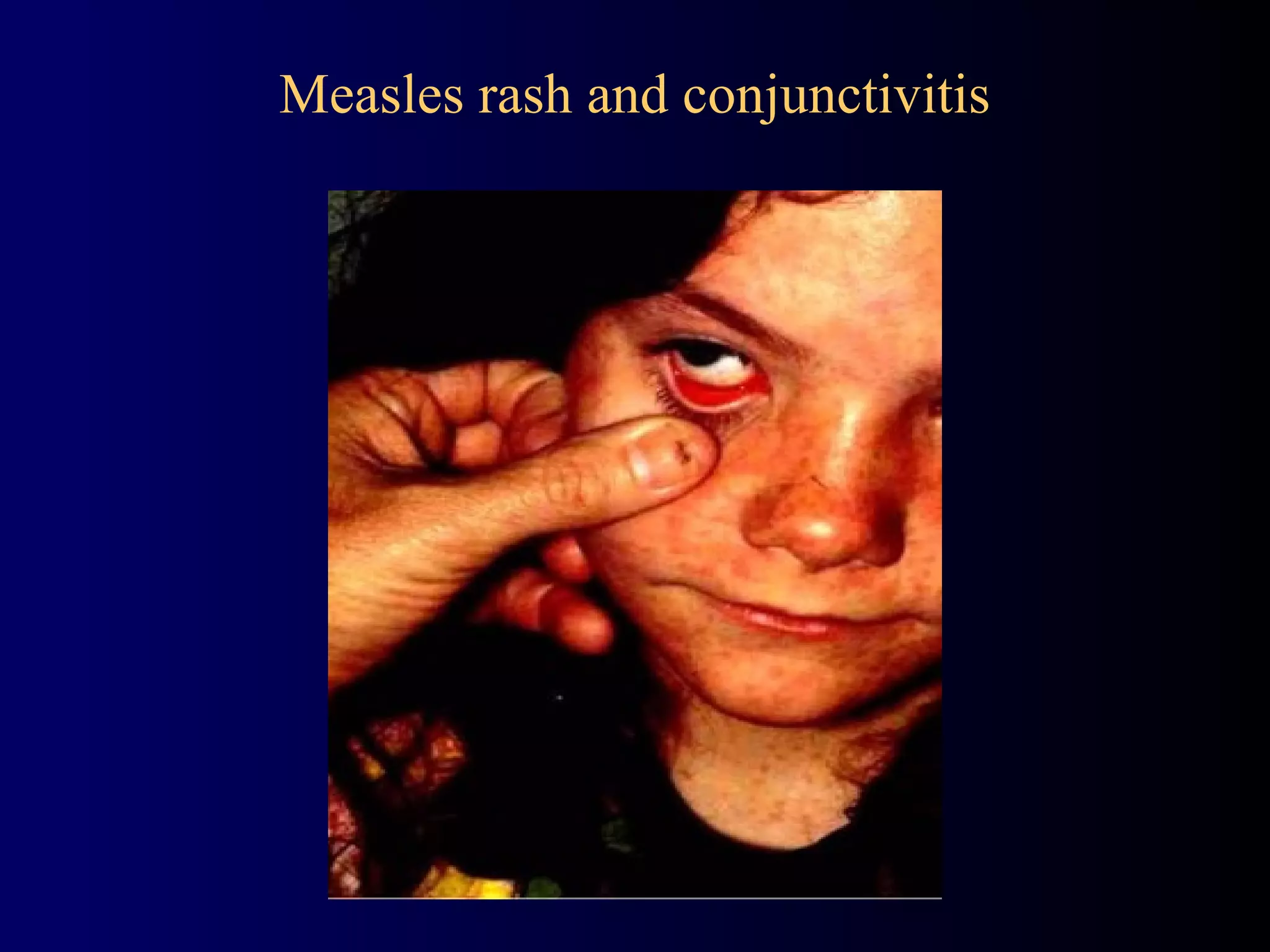
Measles is a highly contagious viral infection with significant historical impacts, causing millions of deaths worldwide before vaccination. It is characterized by symptoms such as fever, cough, coryza, conjunctivitis, and a distinctive maculopapular rash. While there is no specific antiviral treatment, supportive care and vaccination are key in prevention and management of the disease.