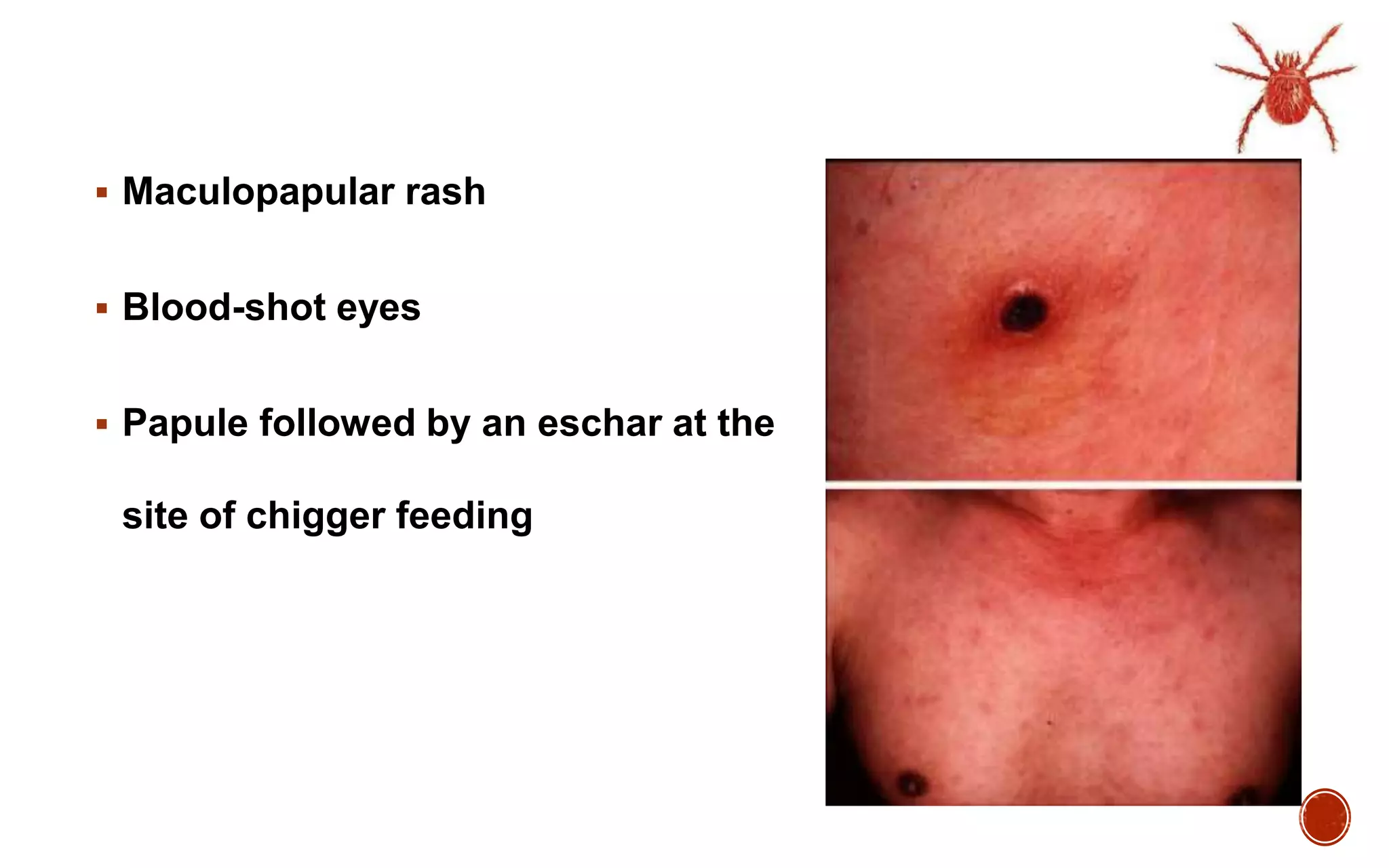
The document discusses scrub typhus, a common rickettsial disease seen in India. It is caused by the bacteria Orientia tsutsugamushi and transmitted by the bites of larval trombiculid mites. Symptoms include fever, rash, and often a characteristic eschar at the bite site. Complications can include pneumonia, meningitis, and multi-organ failure. Diagnosis is made through serology, PCR, or culture. Doxycycline is the treatment of choice, with azithromycin as an alternative, especially in pregnant women and children. Managing complications may require intravenous antibiotics in hospital. Scrub typhus has reemerged as an important cause of febrile