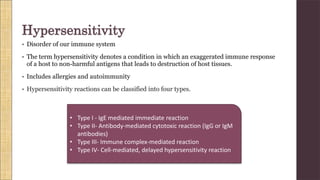
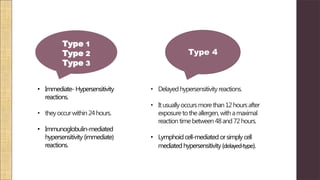
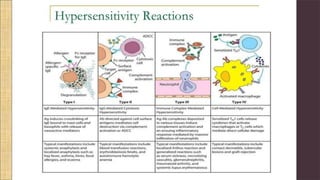
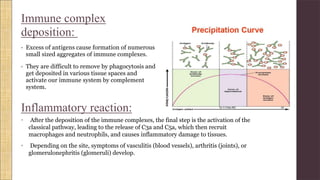
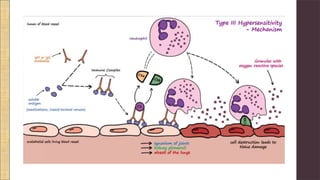
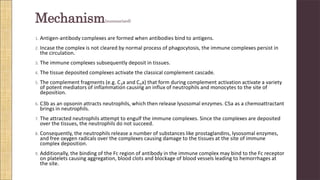
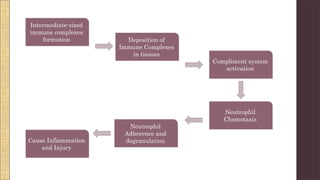
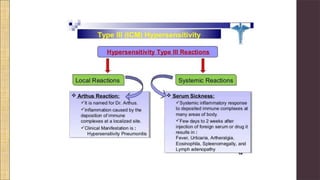
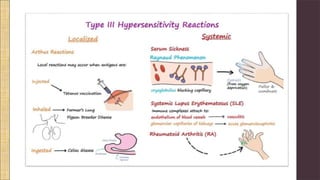
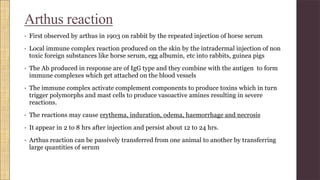
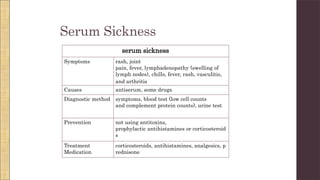
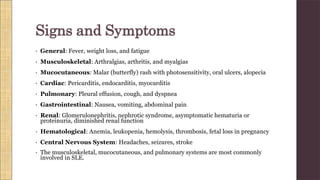
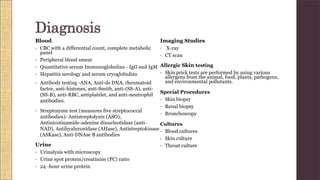
Hypersensitivity Type III involves an exaggerated immune response characterized by the formation of antigen-antibody complexes that lead to tissue damage. Common diseases associated with this reaction include serum sickness, systemic lupus erythematosus, and rheumatoid arthritis, with symptoms manifesting through inflammation in affected tissues. Diagnosis and treatment strategies focus on managing inflammation and addressing the underlying autoimmune disorders.