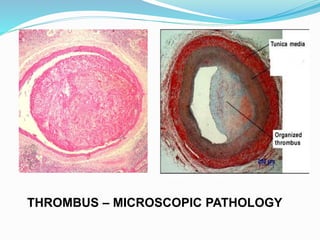
Thrombosis is the formation of a thrombus, a blood clot within the cardiovascular system, which can involve both blood vessel walls and the blood clotting system. It can arise from endothelial injury, abnormal blood flow, or hypercoagulability and is classified based on location, infective agent, and color. The consequences of thrombosis can vary, leading to conditions such as infarction, ischemic necrosis, and in severe cases, sudden death.