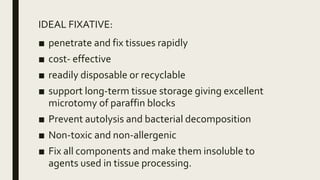
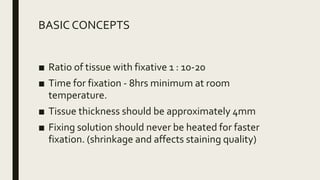
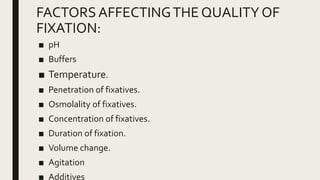
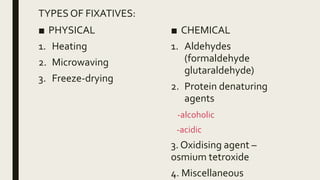
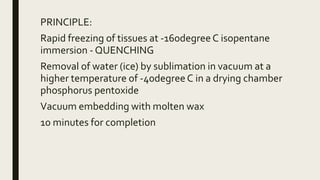
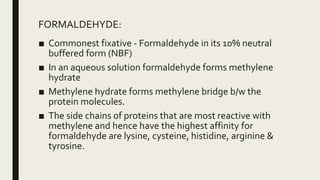
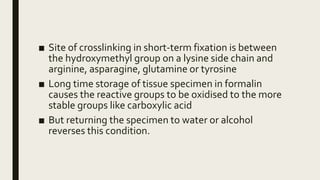
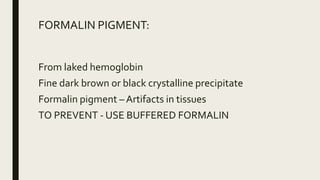
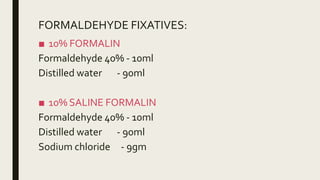
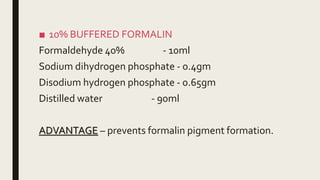
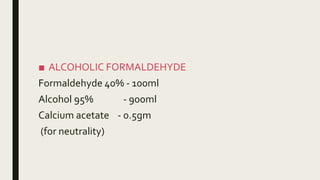
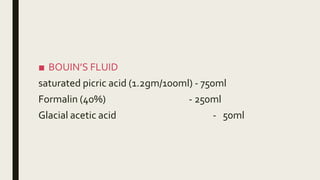
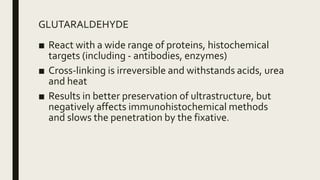
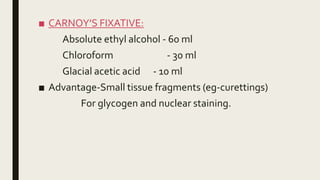
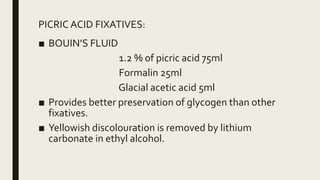
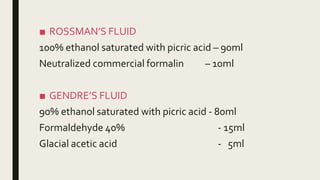
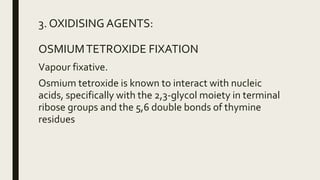
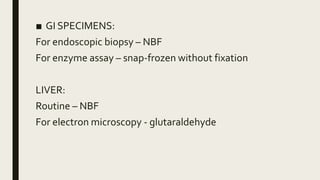
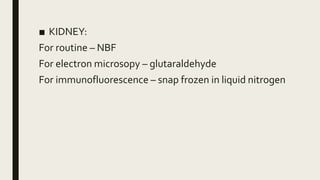
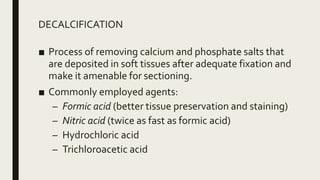
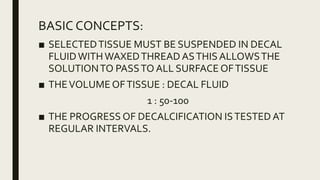
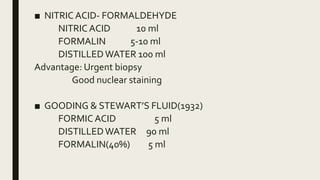
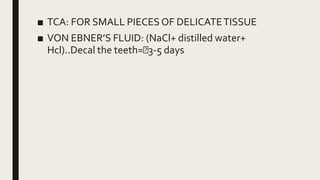
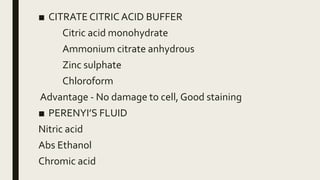
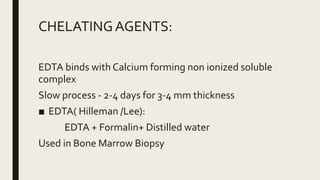
This document discusses histotechniques related to fixation and decalcification of tissues for microscopic examination. It describes the objectives and ideal properties of fixatives, as well as common fixatives used such as formaldehyde, glutaraldehyde, and picric acid. Factors that influence fixation quality like temperature, concentration, and duration are addressed. The document also covers decalcification techniques and factors that affect the decalcification process. Special considerations for fixing different tissues are outlined.