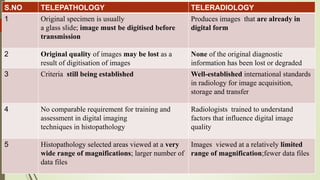
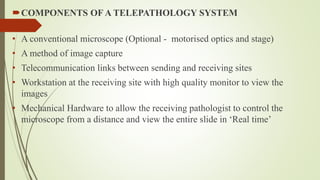
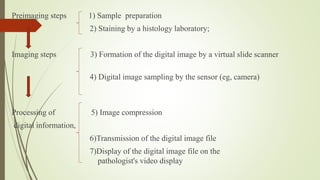
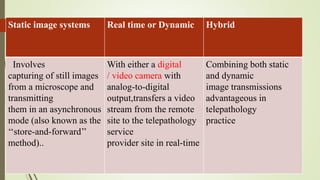
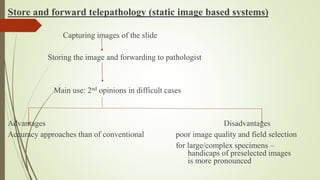
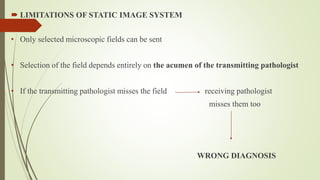
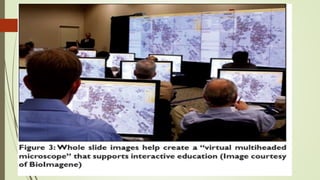
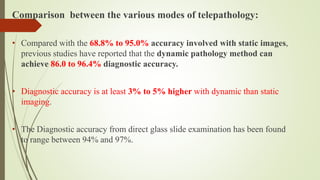
Telepathology involves the digital imaging of pathology specimens and transmitting the images electronically to allow pathologists to render diagnoses remotely. There are three main telepathology systems: static image systems which transmit still images, dynamic systems which provide real-time video transmission, and virtual slide imaging which digitizes entire slides. Telepathology has advantages like allowing expert second opinions and intraoperative consultations, but also challenges like needing standardized criteria and training pathologists in its use to ensure diagnostic accuracy is maintained. While showing promise, telepathology has seen limited adoption in India due to issues around technology, standards, training, and infrastructure.