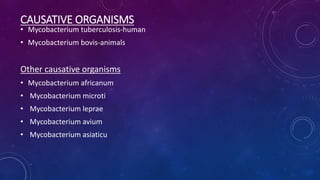
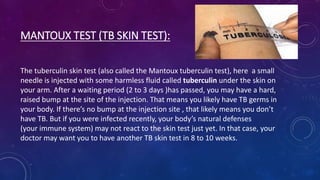
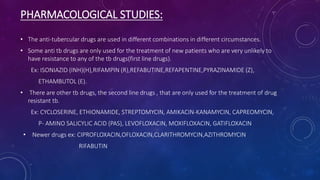
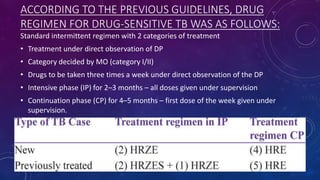
Tuberculosis is caused by the bacterium Mycobacterium tuberculosis. It most commonly affects the lungs. Globally in 2016, there were 10.4 million new cases of TB and 1.7 million deaths from the disease. Risk factors include a weakened immune system, HIV infection, diabetes, silicosis, malnutrition and very young or advanced age. TB spreads through airborne droplets when people with active lung TB cough, sneeze or spit. Diagnosis involves tests such as the tuberculin skin test, TB blood test, chest x-ray, and sputum smear and culture. Standard treatment is 6-9 months of multiple antibiotic drugs, usually including isoniazid and rifampin.