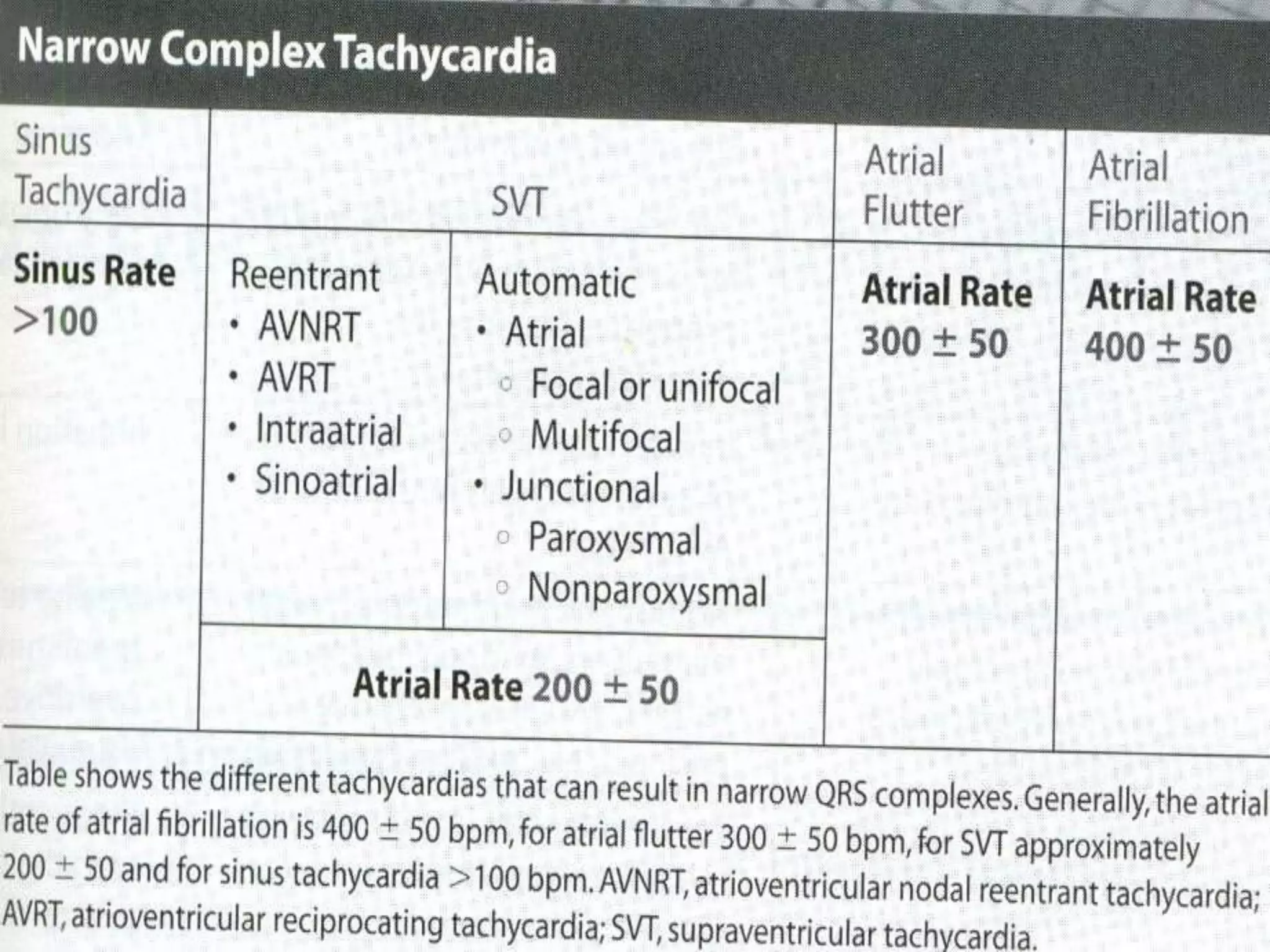
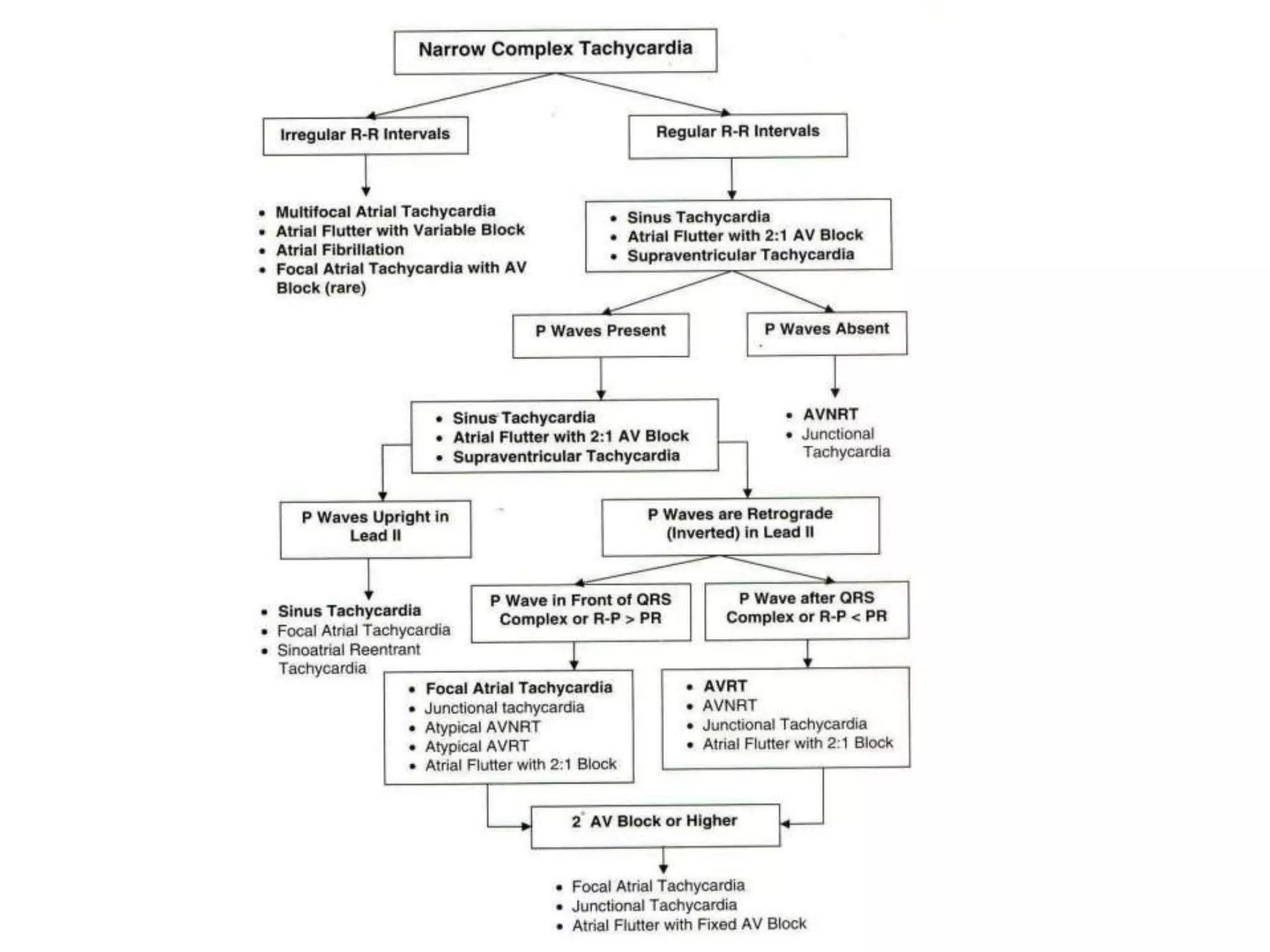
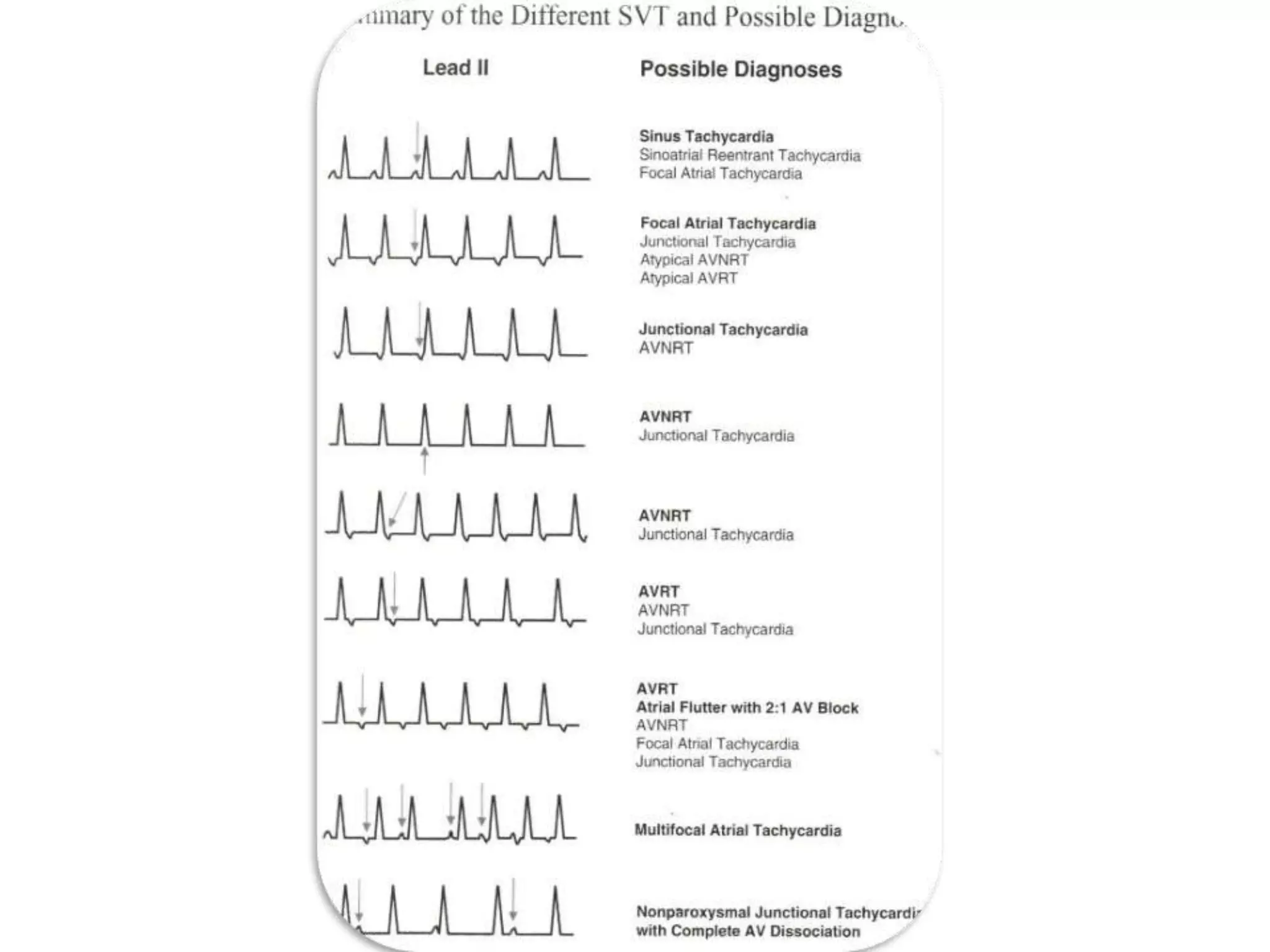
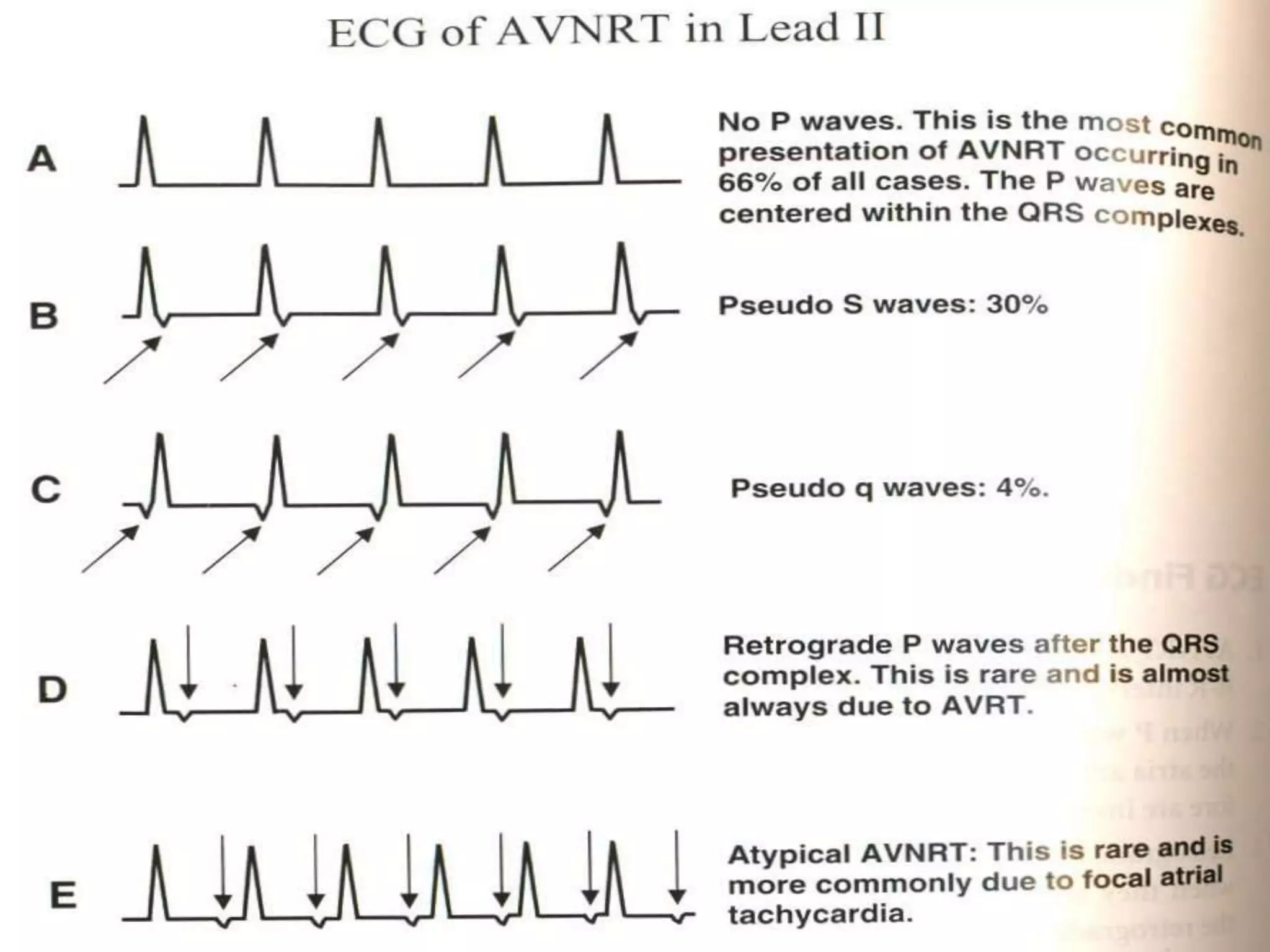
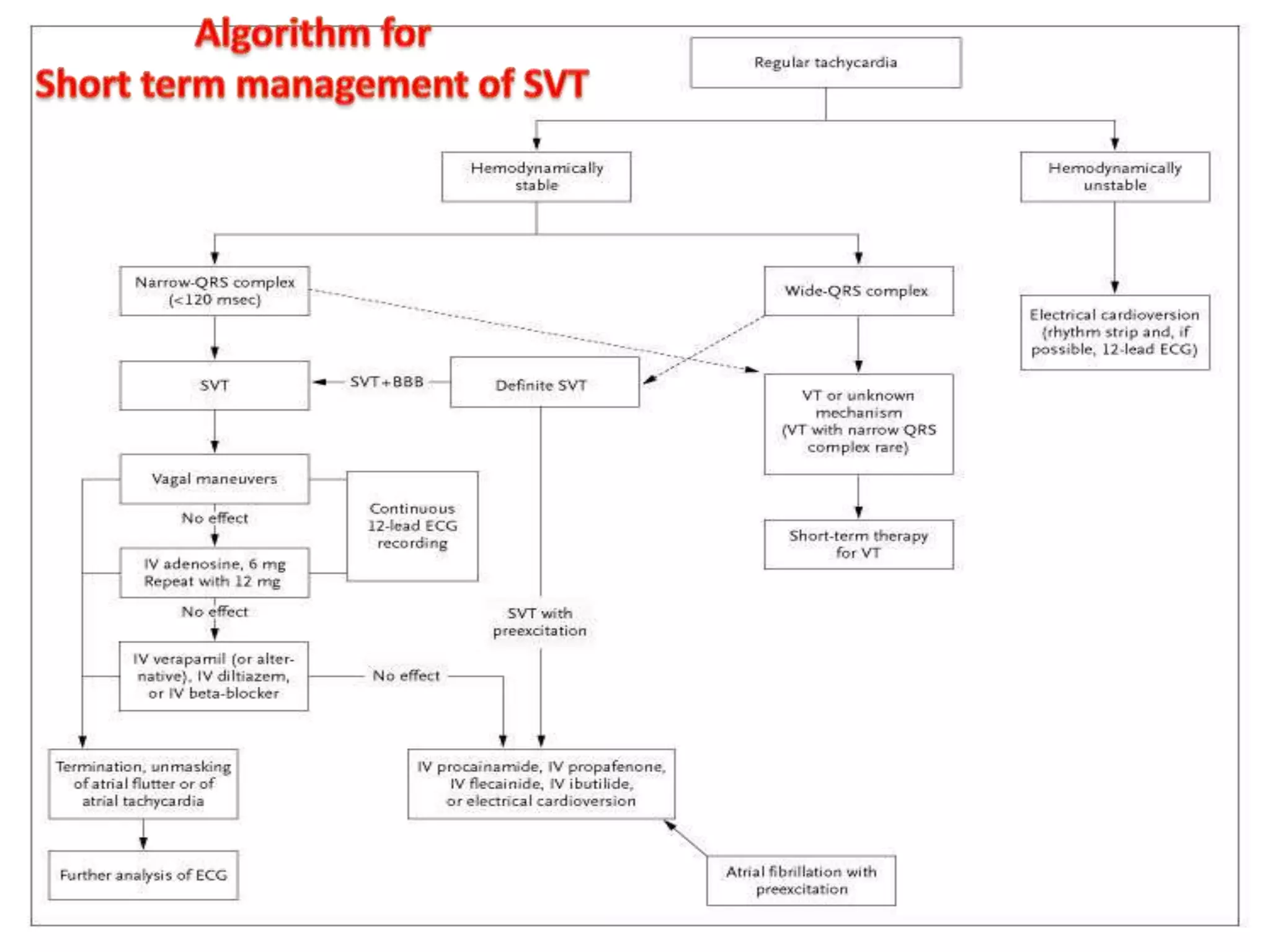
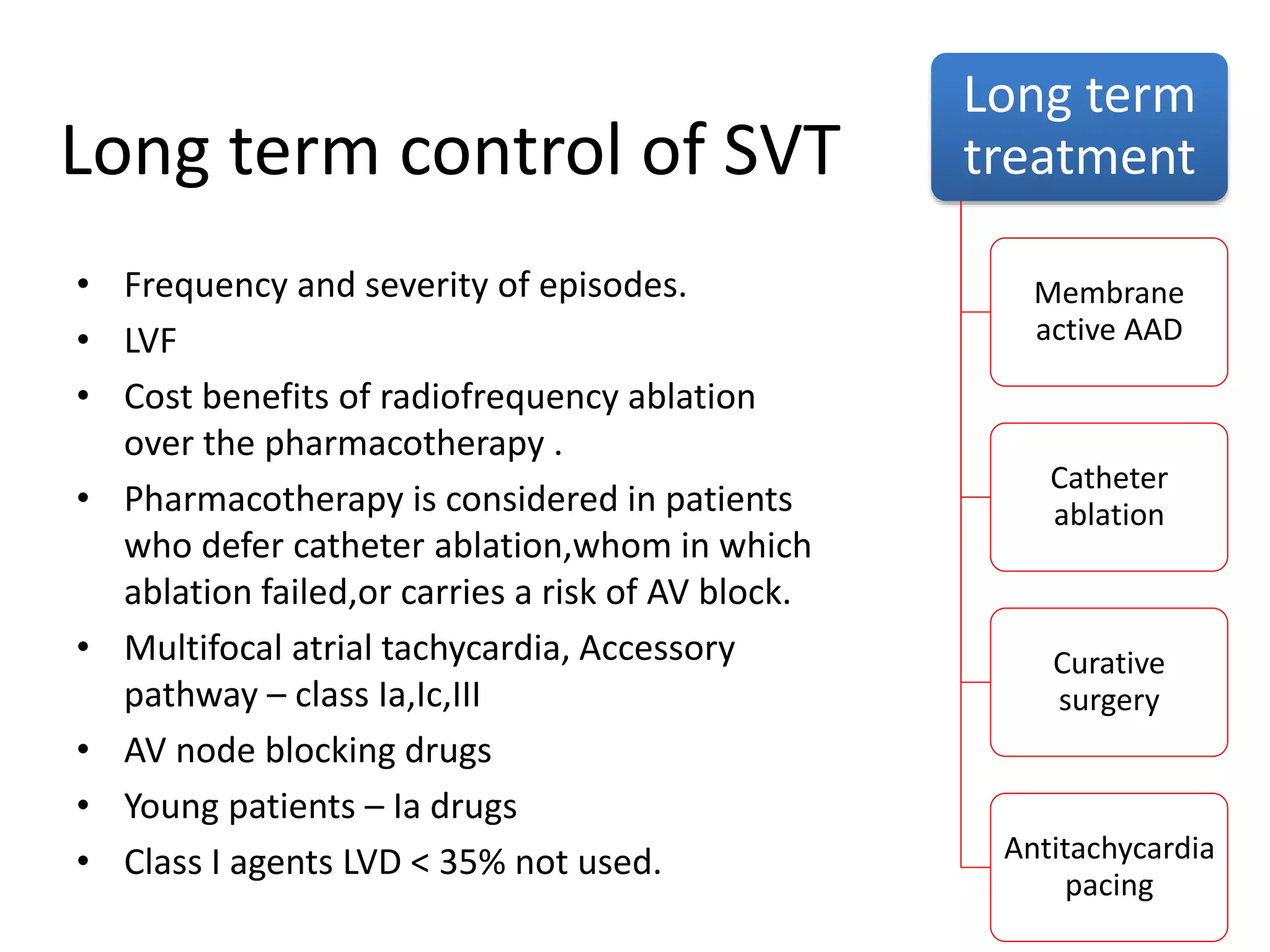
This document provides an overview of approaches to evaluating and treating narrow complex tachycardia. It outlines steps to determine the mechanism, including examining P wave morphology and relationship to QRS. Common types discussed are AV nodal reentrant tachycardia (AVNRT), atrioventricular reentrant tachycardia (AVRT), focal atrial tachycardia, and junctional tachycardias. Treatment options are also summarized, including vagal maneuvers, adenosine, calcium channel blockers, beta blockers, antiarrhythmic drugs, catheter ablation, and pacemaker therapy.