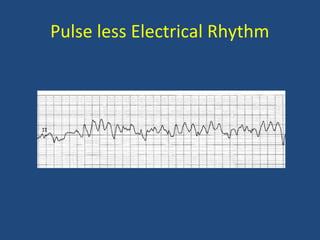
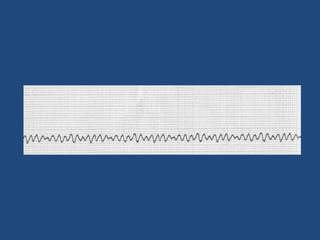
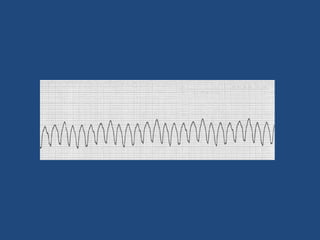
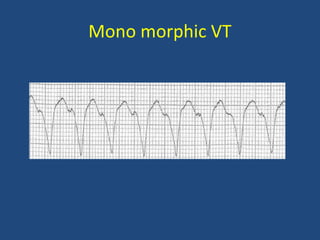
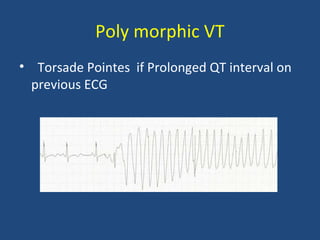
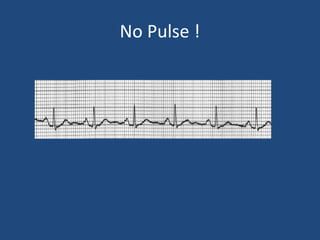
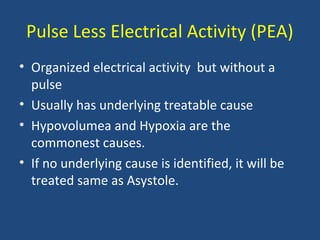
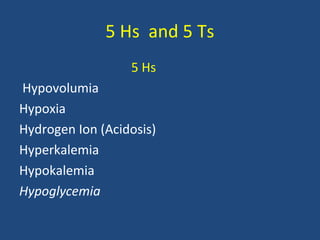
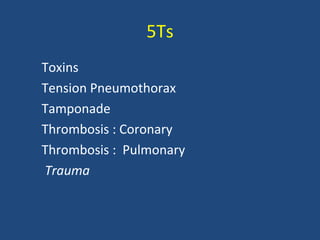
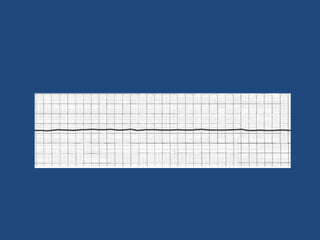
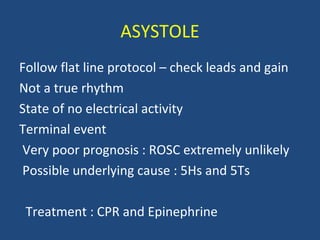
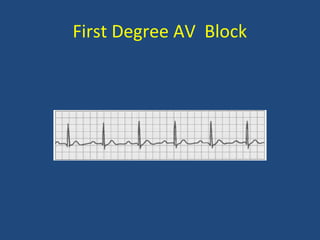
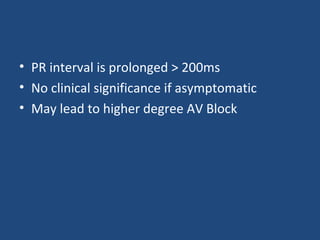
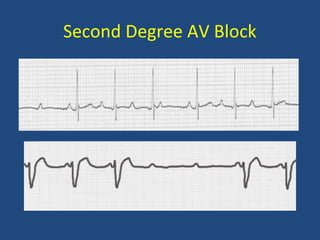
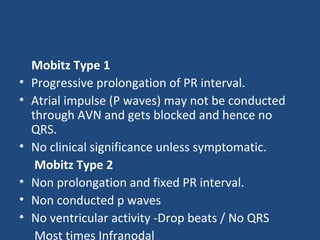
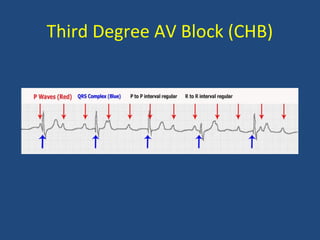
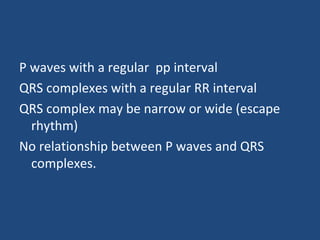
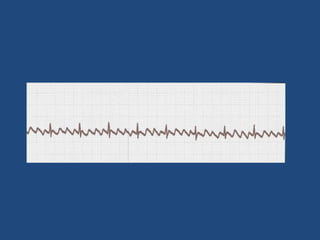
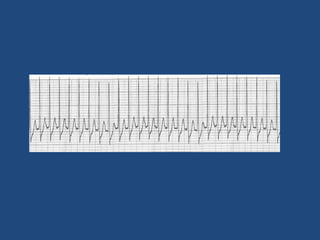
This document provides an overview of various arrhythmias that may be encountered in ACLS situations. It discusses pulseless rhythms like ventricular fibrillation and ventricular tachycardia, which require immediate defibrillation. It also covers pulseless electrical activity, asystole, and various bradyarrhythmias and tachyarrhythmias like atrial fibrillation and atrial flutter. For each arrhythmia, it outlines characteristics like heart rate, pulse presence, ECG patterns, potential causes, and recommended treatment approaches. The goal is to help providers quickly recognize rhythms and deliver the appropriate life-saving therapy in cardiac arrest situations.