This document provides an overview of tachyarrhythmias, including:
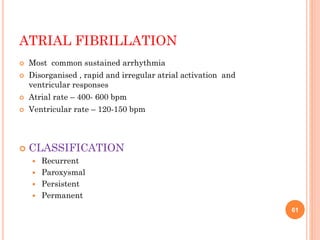
- Definitions of tachyarrhythmias as disturbances in heart rhythm over 100 beats per minute.
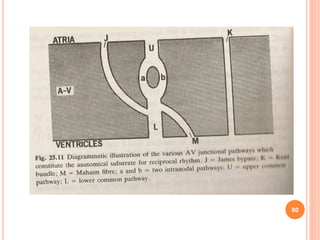
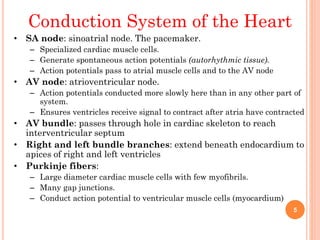
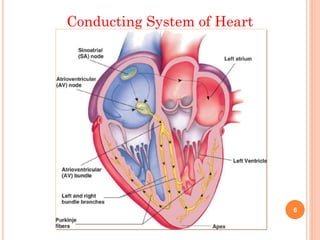
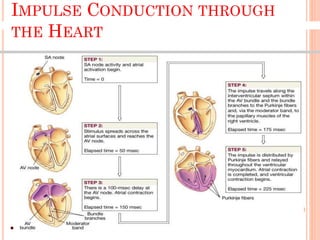
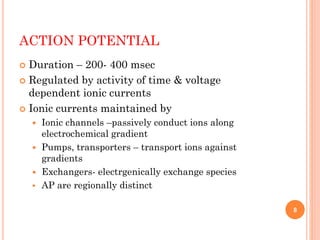
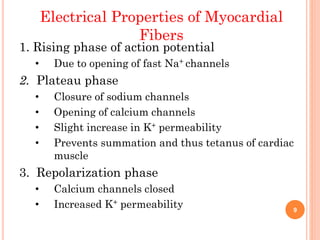
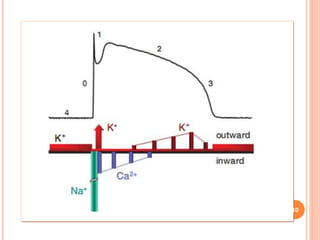
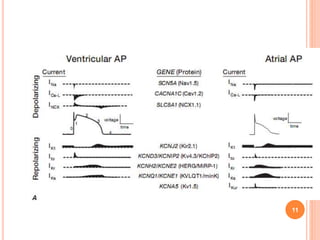
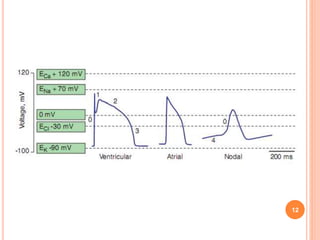
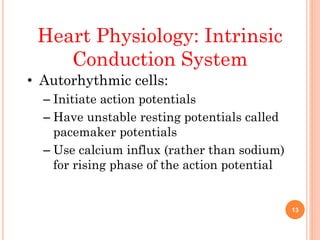
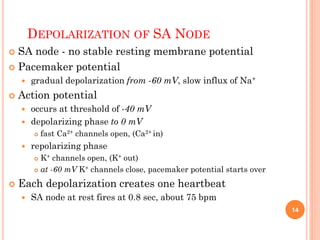
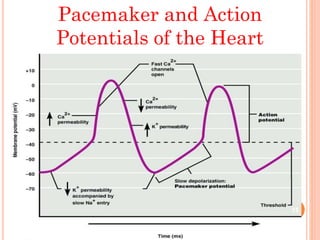
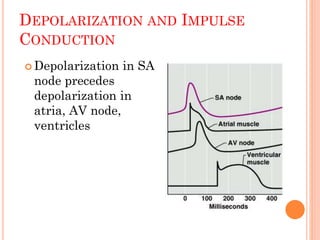
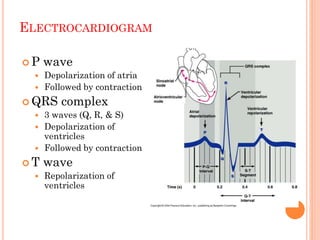
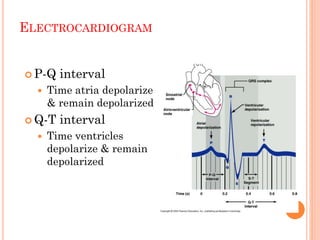
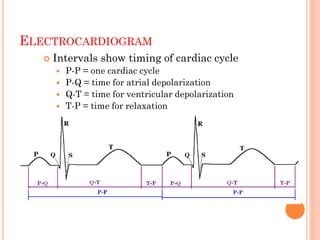
- Anatomy and electrophysiology of the heart's conduction system.
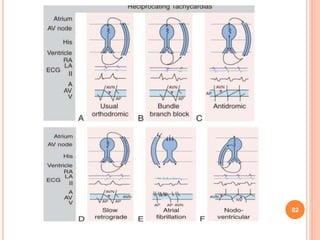
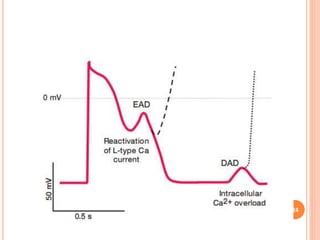
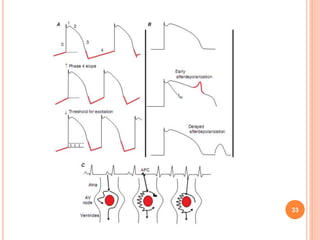
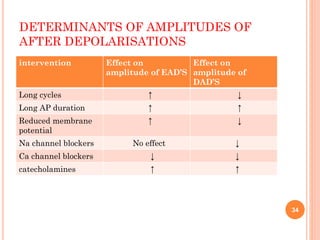
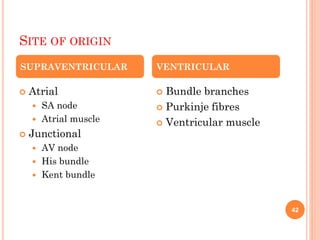
- Mechanisms of arrhythmogenesis including disorders of impulse formation and conduction.
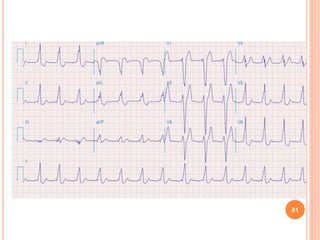
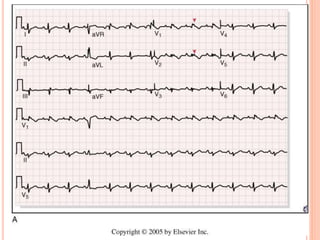
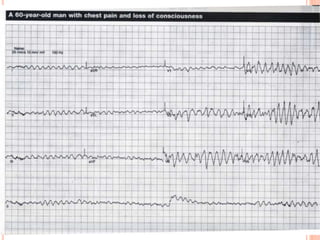
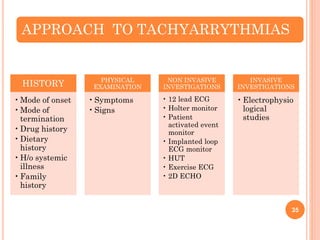
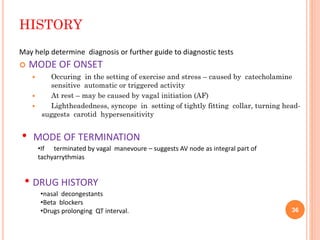
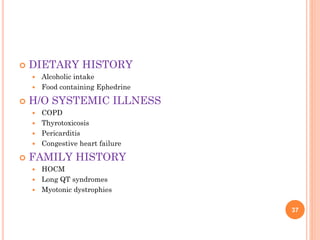
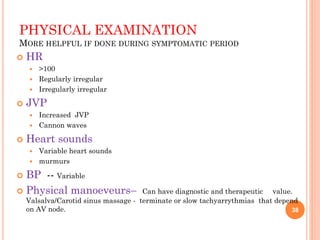
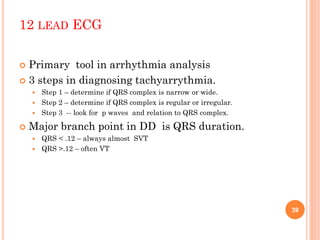
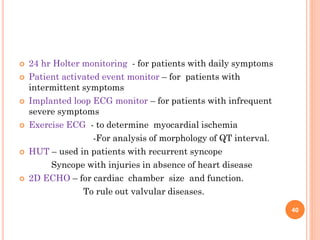
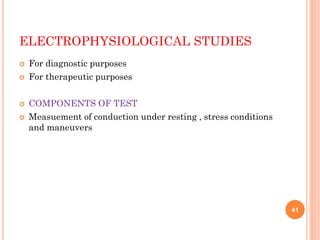
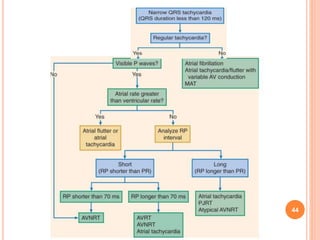
- Diagnostic approach involving history, physical exam, ECGs, monitoring, and invasive studies.
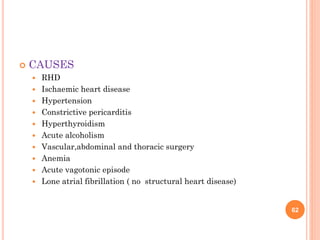
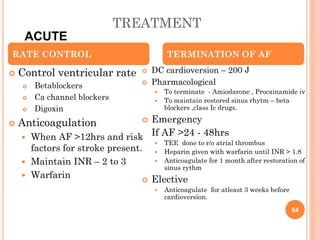
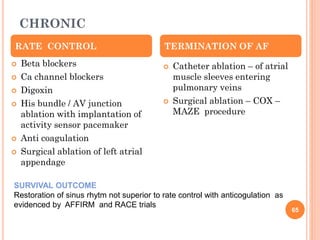
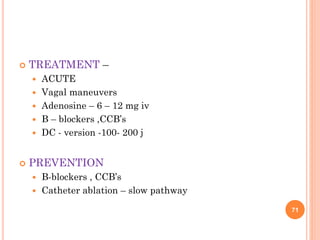
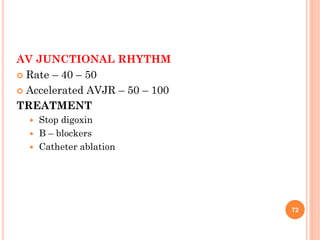
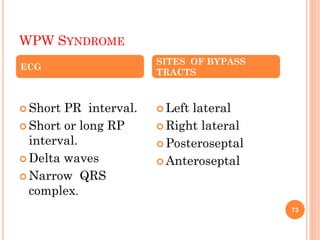
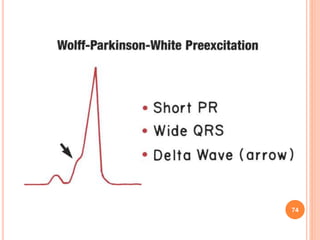
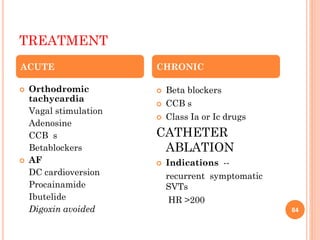
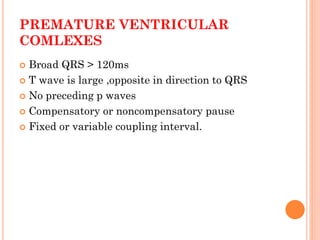
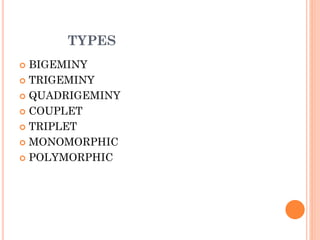
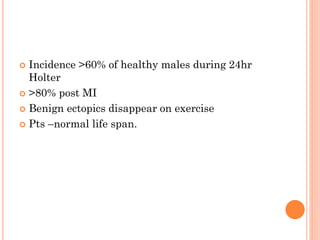
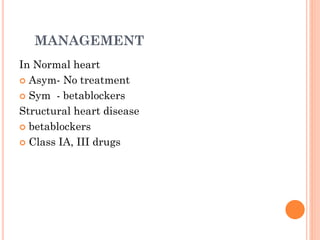
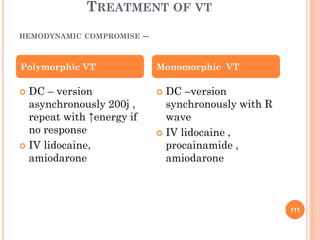
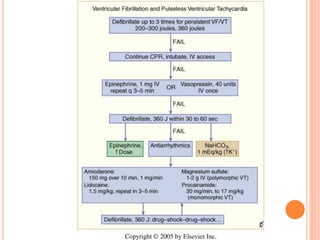
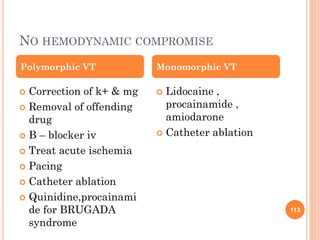
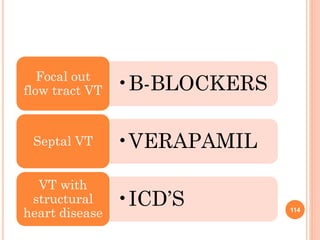
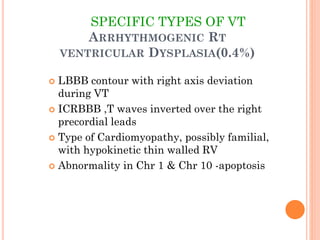
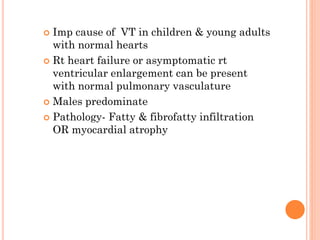
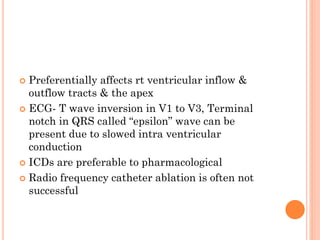
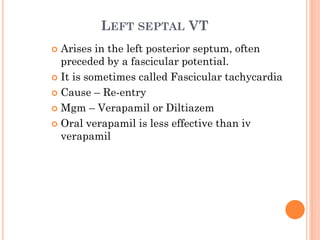
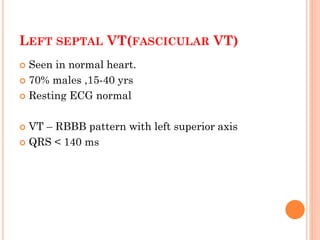
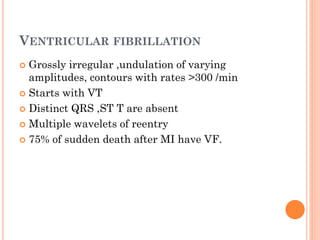
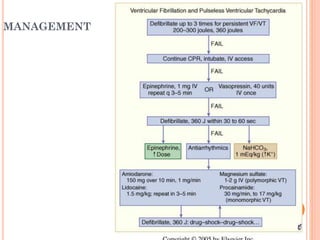
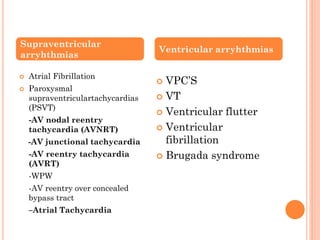
- Treatment modalities including antiarrhythmic drugs and ablation procedures for various specific arrhythmias like atrial fibrillation, supraventricular tachycardias, and ventricular arrhythmias.

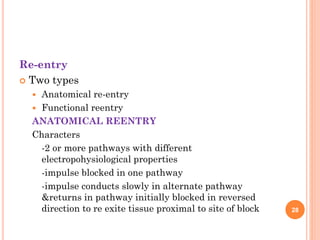
![ For re entry to occur anatomical length of circuit
should be greater than reentrant wave length
Conditions that depress conduction velocity &
refractory period promote development of re
entry[λ = c.v x rp]
Sustained reentry occurs due to excitable gap
between activating head & recovery tail.
30](https://image.slidesharecdn.com/rktacy-140506091240-phpapp01/85/tachyarrythmias-d-30-320.jpg)
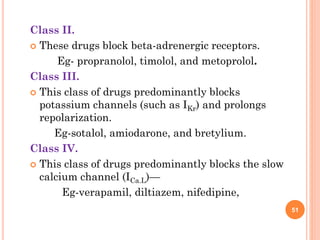
![ANTIARRYHTHMIC DRUGS
Class IA.
This includes drugs that reduce V.max (rate of rise of action
potential upstroke [phase 0]) and prolong action potential
duration
Eg-quinidine, procainamide, disopyramide.
Class IB.
This class of drugs does not reduce V.max and shortens
action potential duration—
Eg-mexiletine, phenytoin, and lidocaine.
Class IC.
This class of drugs can reduce V.max, primarily slow
conduction, and prolong refractoriness minimall
Eg-flecainide, propafenone, and moricizine. 50](https://image.slidesharecdn.com/rktacy-140506091240-phpapp01/85/tachyarrythmias-d-50-320.jpg)