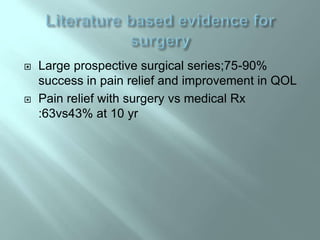
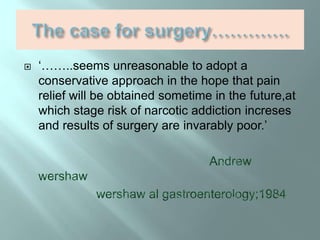
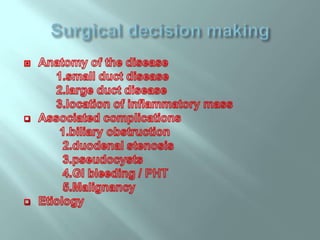
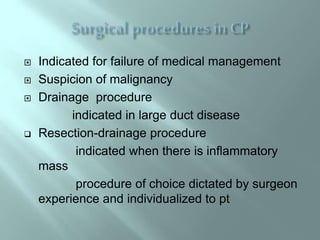
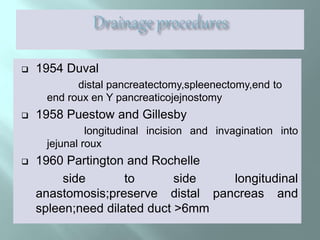
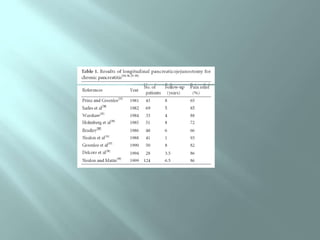
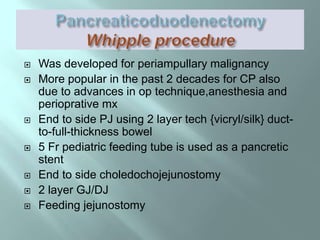
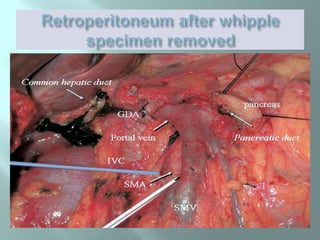
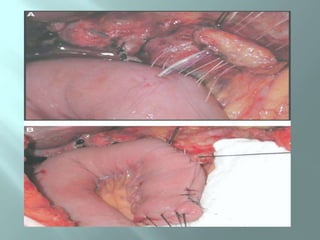
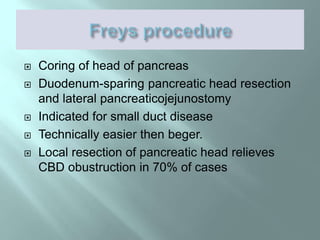
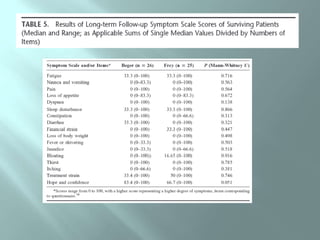
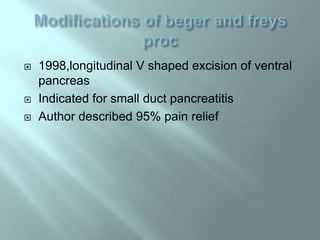
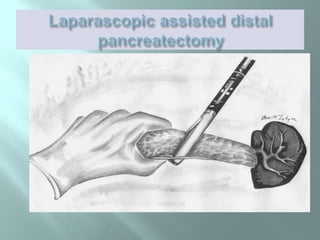
This document discusses chronic pancreatitis, including its definition, causes, symptoms, diagnostic tests, and surgical treatment options. It notes that chronic pancreatitis is characterized by irreversible morphological changes and permanent loss of pancreatic function. The main indications for surgery are intractable pain and complications. Surgical options include drainage procedures like longitudinal pancreaticojejunostomy or cyst-enterostomies, as well as resections like Whipple procedure or distal pancreatectomy. The goals of surgery are pain relief, control of complications, and improved quality of life. While surgery provides sustained pain relief in over 85% of patients, outcomes may be complicated by associated issues like portal hypertension.
![ Continuous inflammatory disease of pancreas
characterised by irreversible morphologic
changes [[irregular fibrosis, acinar and islet
cells loss,inflammatory infiltrates,stone
formation]]of both the parenchyma and
ducts;typically coupled with permanent loss of
function +/-pain](https://image.slidesharecdn.com/surgeryinchronicpancreatitisv-140525002846-phpapp01/85/Surgery-in-chronic-pancreatitis-2-320.jpg)
![ Alcohol;60-70% of all cases in developed
countries {6-12 yr history of 150-175 g/day}
Obstruction of pancratic duct;pancreas
divisum,post traumatic stricture,tumours
Cystic fibrosis[CFTR mutation]
Tropical pancreatitis
Autoimmune
Hypercalcemia
Hyperlipidemia
idiopathic](https://image.slidesharecdn.com/surgeryinchronicpancreatitisv-140525002846-phpapp01/85/Surgery-in-chronic-pancreatitis-4-320.jpg)
![ TESTS OF
STRUCTURE
1.ERCP
2.EUS
3.MRI AND MRCP
4.CT scan
5.X ray abdomen
6.USG abdomen
TESTS OF
FUNCTION
1.S. Glucose
2.S.Trypsinogen
3.Fecal elastase
4.Fecal chymotrypsin
5.Fecal fat[72 hr
collection]
6.Secretin pancreatic
stimulation test with
duodenal intubation](https://image.slidesharecdn.com/surgeryinchronicpancreatitisv-140525002846-phpapp01/85/Surgery-in-chronic-pancreatitis-7-320.jpg)
![ Pain –commonest indication[[[70-90%]]]
Mass/suspicion of malignancy
Biliary obstuction
Duodenal stenosis
Pseudocysts
Internal pancreatic fistulae
Vascular problems](https://image.slidesharecdn.com/surgeryinchronicpancreatitisv-140525002846-phpapp01/85/Surgery-in-chronic-pancreatitis-13-320.jpg)
![ Patients presented with complications;early
surgery
For pain relief
.early surgery [<4 yrs ]may delay progress
of exocrine/endocrine insufficiency[alc CP]
Ann surg 1999
.early surgery in NACP/trop CP improves
nutitrional status,weight gain,decrased insulin
requirement.
Controversies:how early what surgery:drainage or
resection?](https://image.slidesharecdn.com/surgeryinchronicpancreatitisv-140525002846-phpapp01/85/Surgery-in-chronic-pancreatitis-21-320.jpg)
![ Inflamed and enlarged pancreatic head
Requires resection
1.Whipple
2.Beger[duodenum preserving pancreatic
head resection]
3.Frey](https://image.slidesharecdn.com/surgeryinchronicpancreatitisv-140525002846-phpapp01/85/Surgery-in-chronic-pancreatitis-24-320.jpg)

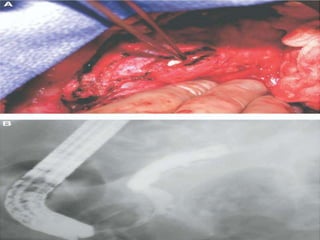
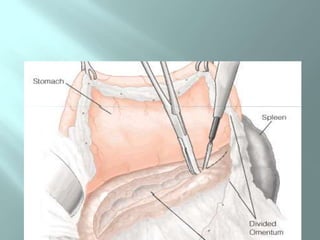
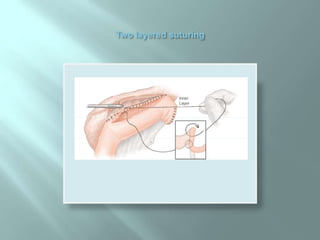
![ Duodenum-sparing pancreatic head resection
C/I in suspected pancretic cancer
Portal vein freed,neck divided
Longitudinal pancreaticojejunostomy
Frozen section to rule out malignancy[5%]](https://image.slidesharecdn.com/surgeryinchronicpancreatitisv-140525002846-phpapp01/85/Surgery-in-chronic-pancreatitis-33-320.jpg)

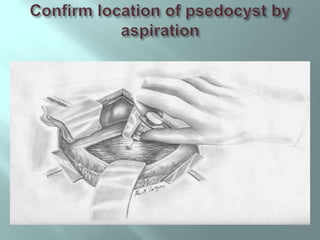
![ Psedocyst complicates CP in 30% to 40% of
pts
Surgery indicated for pts with symtomatic
pseudocysts who are either not candidate or
have failed an initial attempt at
transampullary,transgastric,or transcutaneous
drainage
septated cyst with elevated fluid CEA and CA
15-3 levels treated by resection.[? Neoplasm]
](https://image.slidesharecdn.com/surgeryinchronicpancreatitisv-140525002846-phpapp01/85/Surgery-in-chronic-pancreatitis-42-320.jpg)
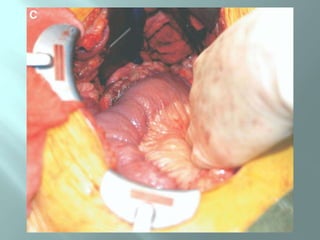
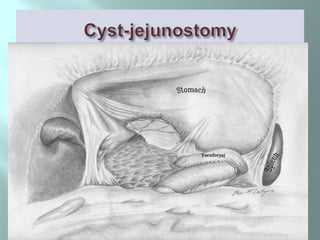
![ Cyst-gastrostomy/duodenostomy
Roux-en-Y cyst-jejunostomy [simpler]
For small multiple cysts of pancreatic head-
Whipple proc
For cyst of pancreatic tail – distal
pancreatectomy](https://image.slidesharecdn.com/surgeryinchronicpancreatitisv-140525002846-phpapp01/85/Surgery-in-chronic-pancreatitis-43-320.jpg)
![ 1995-2009 [[n=170]]
Pain is the main indication 90%
pain duration 1-30 yrs
Biliary obstruction alone 10%
NACP: 95 ; Alc CP ;75
DRAINAGE PROCEDURE …………….115
LPJ ………………………………….62
LPJ+BILIARY BYPASS …………….30
CYST-ENTEROSTOMIES …………23
RESECTIONS…………………………….19
WHIPPLES ………………………….11
WHIPPLES+LPJ …………………….3
DISTAL PANCREATECTOMY …….5](https://image.slidesharecdn.com/surgeryinchronicpancreatitisv-140525002846-phpapp01/85/Surgery-in-chronic-pancreatitis-51-320.jpg)
![ Pain relief and quality of life issues are the
main concern in pts of chronic pancreatitis
undergoing treatment
Surgery is indicated for relief of intractable pain
and complications associated with CP
Failure of nonsurgical treatment and presence
of complications influence timing and need for
surgical intervention[[jury is still out:early surgery for
mild to moderate pain]]](https://image.slidesharecdn.com/surgeryinchronicpancreatitisv-140525002846-phpapp01/85/Surgery-in-chronic-pancreatitis-52-320.jpg)