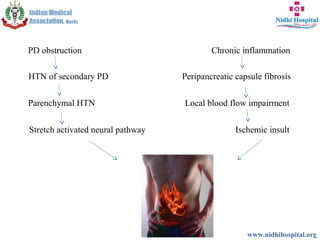
The document discusses surgical management of chronic pancreatitis. It describes various surgical procedures for treating chronic pancreatitis including resection procedures like Whipple procedure, drainage procedures like Puestow's procedure, and hybrid procedures like Frey procedure. Studies have shown that duodenum-preserving pancreatic head resection procedures and longitudinal pancreaticojejunostomy provide better postoperative outcomes and pain control compared to resection procedures while preserving exocrine and endocrine function. The document concludes that surgery is effective for relieving pain in chronic pancreatitis and duodenum-preserving pancreatic head resection procedures have advantages over other surgical options.