This document discusses the presentation, diagnosis, and management of chronic pancreatitis. Key points include:
- Abdominal pain is the most common symptom, often worsened by eating and relieved by forward leaning. Weight loss, steatorrhea, and diabetes can also occur.
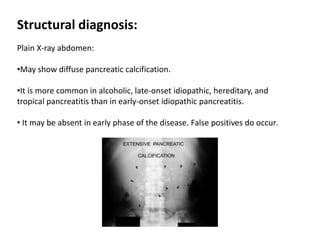
- Diagnosis involves functional tests like fecal fat tests and glucose tolerance tests, as well as imaging like CT, MRI, and EUS to detect structural changes in the pancreas.
- Treatment focuses on managing pain, replacing lost exocrine function with pancreatic enzyme supplements, treating diabetes, and occasionally intervening for complications like pseudocysts or stones. Lifestyle changes and medication are used alongside enzyme replacement therapy.