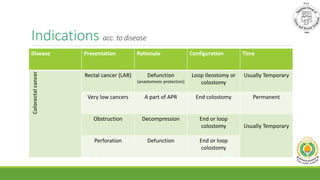
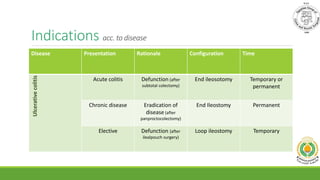
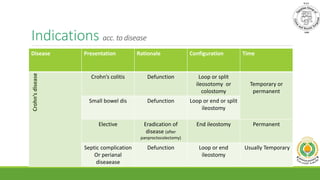
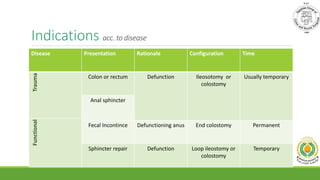
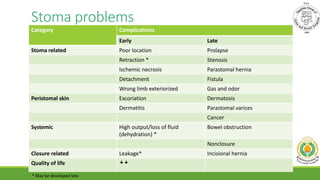
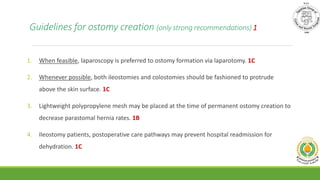
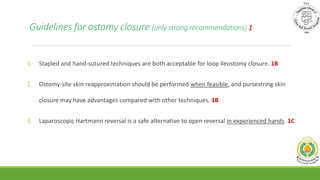
Loop ileostomy or loop colostomy can be used to divert fecal streams and protect colorectal anastomoses based on indications from various diseases and procedures. Complications occur in 21-70% of cases, relating to the stoma, peristomal skin, or systemic issues. Guidelines recommend techniques to decrease complications like laparoscopy, protruding stomas, and mesh reinforcement. While some studies found ileostomy had fewer hernias and prolapses, meta-analyses show no clear preference between ileostomy and colostomy. Alternative options like ghost ileostomy or transanal decompression tubes may help avoid stomas in some cases.