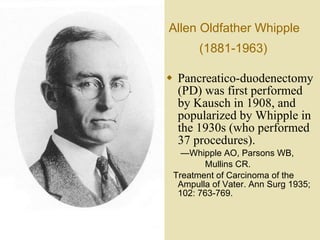
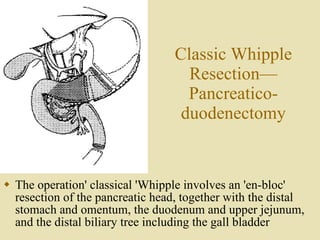
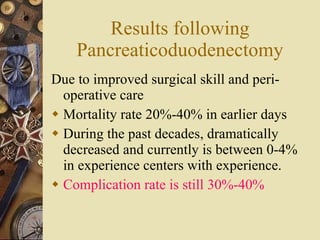
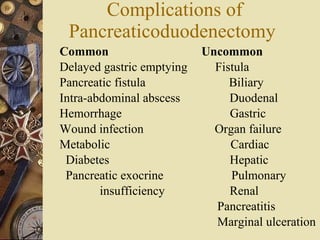
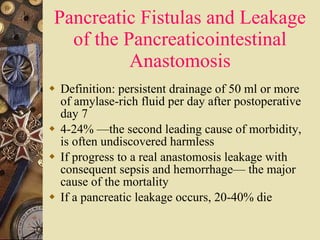
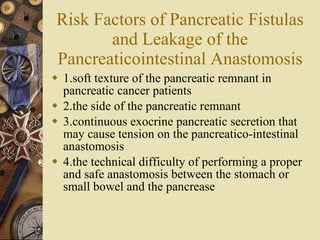
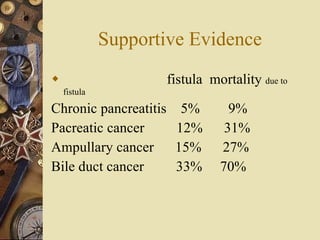
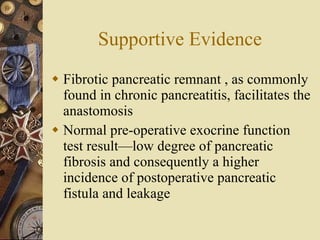
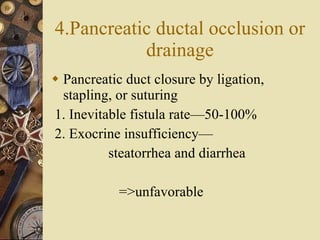
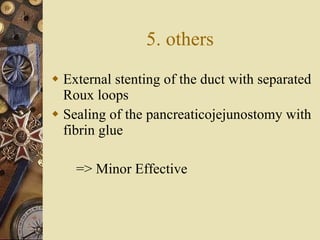
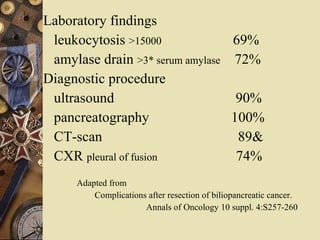
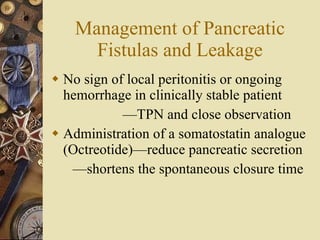
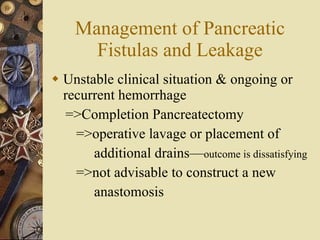
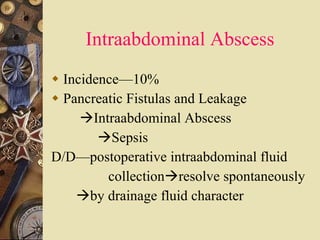
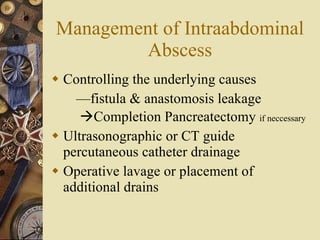
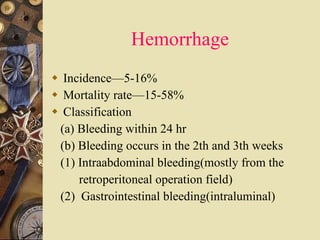
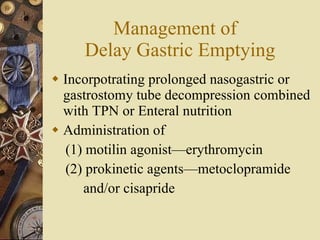
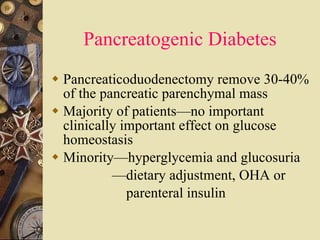
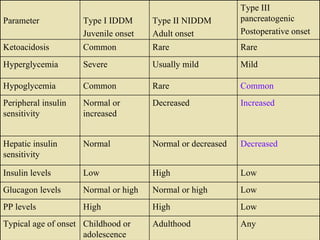
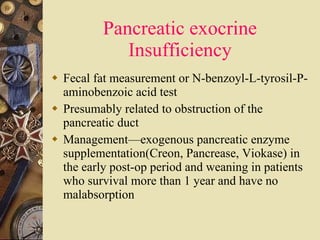
The document discusses complications that can occur after a Whipple procedure (pancreaticoduodenectomy), including pancreatic fistulas, delayed gastric emptying, hemorrhage, and diabetes. It provides details on the risk factors, symptoms, diagnosis, and management of each complication. The Whipple procedure has become safer in recent decades but still carries risks of complications in 30-40% of patients.